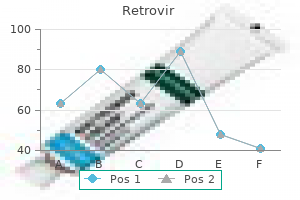
Retrovir dosages: 300 mg, 100 mg
Retrovir packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Retrovir 100 mg overnight delivery
Care is taken to drape out a large surgical area in case a more extensile method is necessary. Preoperative Planning Thorough preoperative planning is the vital thing to a successful reconstruction. In all cases of revision, stemmed and constrained implants (or sometimes a hinged prosthesis) have to be considered and must be available. An intensive synovectomy and d�bridement of the medial and lateral gutters are critical for decompression of the joint. In knees with severe ankylosis, techniques such as the quadriceps snip, lateral release, and tibial turbercle osteotomy are helpful for publicity. The surgeon should know the implications of each of those releases and restore or reconstruct them properly at the end of the procedure. The bone defect is addressed by means of cement (smaller lesions), metal augments, or structural grafts. The critical issues are to restore joint line, obtain appropriate alignment, and attain ligamentous balancing. Reconstruction additionally aims at restoring a steady platform for positioning and fixation of the components. Careful preoperative planning is required to have the flexibility to handle bone loss encountered on the time of arthroplasty. Most cases of knee revision with bone loss could be addressed with the usage of a long-stem prosthesis and metallic augments. For most techniques, the largest femoral augments enable for restoration of eight to 10 mm of bone defect. The use of cemented stacked augments for filling defects up to 30 mm has been reported. The distal femoral minimize is freshened to present a secure platform for the new prosthesis. Determining proper femoral component rotation is crucial to a successful reconstruction. Other secondary guides include the proximal tibia and the femoral intercondylar line. Malrotation of the femoral part can also exaggerate the severity of bone loss. The rest of the reconstruction varies according to the revision knee system getting used, however should follow a scientific approach. Some implants have trials with slots, which allows for extra exact sizing and preparation for modular augments. A stemmed trial femoral element with the mandatory augments is assembled and inserted. The definitive prosthesis is assembled and cemented into place in the standard fashion. Areas of bony sclerosis should be d�brided to punctate bleeding with the assist of a high-speed burr. The femur is ready with the revision instrumentation specific to the implant system, paying consideration to joint line restoration, rotation, and restoration of the posterior condylar offset. The use of stemmed implants allows for distribution of joint stresses and virtually always is required in cases of revision surgery with bone loss. The new femoral part is cemented into place separately, and the cement is allowed to harden underneath direct vision. The major advantage of this method is that it permits for restoration of bone stock. Prepare the femur utilizing the revision instrumentation specific to the system getting used. Once the femur is ready, insert a stemmed trial femoral component, with or with out wedges, onto the femur. Before final impaction of the trial part, tightly pack the bone chips across the stems and the posterior condyles. Impacting the trial prosthesis into place will successfully form the model new distal femur. The new stemmed femoral part is cemented separately to minimize the possibility of part malposition. The attachments of the collateral ligaments are preserved by a thin shell of bone following removing of the femoral implant.
Purchase retrovir 100mg line
Such closure could lessen the possibility of lateral spur formation, add stability, and speed therapeutic. [newline]Any loss of discount suggests instability and prompts the necessity for operative intervention. A posterior or posterolateral metaphyseal bone spur incessantly varieties postoperatively. Warning the mother and father initially of the probability of the prevalence can scale back nervousness later. Postoperative bone spur Postoperative swelling Placing felt over the minimize, bend ends of the wires onto the pores and skin decreases the danger of pores and skin swelling over or pressing into their sharp suggestions while in the forged. Delayed union and nonunion this happens more commonly in fractures treated nonoperatively. Cubitus valgus and tardy ulnar nerve palsy Premature closure of the lateral physis might lead to gradual deformity because the medial aspect continues to grow. Nerve signs can take years to develop; subsequently, patients should be recommended about indicators and symptoms of ulnar nerve stretch. Cubitus varus Unstable fractures handled nonoperatively can displace proximally and laterally, allowing the elbow to drift right into a varus place. Although some have proven enough healing by 3 weeks, a period of four to 6 weeks is generally required; the decision should be based on radiographic evidence of early callus. Tardy ulnar nerve palsy can develop slowly with progressive valgus deformity following untimely growth arrest or nonunion. Approximately 10% have minor loss of extension (10 to 15 degrees) at 1 to 2 years. Prevention and remedy of nonunion of slightly displaced fractures of the lateral humeral condyle in youngsters: an end-result study. Fractures of the lateral humeral condyle: role of the articular hinge in fracture stability. Usefulness and accuracy of arthrography in management of lateral humeral condyle fractures in youngsters. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. Fortunately, these tend to clean over time and are rarely symptomatic; thus, they often require no treatment. Delayed union and nonunion are more widespread with nonoperative treatment than with surgical therapy. Malunion might occur in unstable fractures handled nonoperatively or in these with premature growth arrest. Avascular necrosis is extra common after operative therapy than nonoperative management and is likely as a end result of extreme posterior stripping that disrupts the epiphyseal blood provide. Chapter three Open Reduction and Internal Fixation of Fractures of the Medial Epicondyle Brian G. Untreated displaced fractures could lead to continual medial elbow instability and even recurrent elbow dislocations. More generally, a fall on an outstretched arm causes an avulsion of the medical epicondyle by way of pressure generated by stretch of the muscle tissue attaching to it. Considerable force utilized to the arm may trigger elbow dislocation and related disruption of the ulnar collateral ligament. This ligament, the principal stabilizing ligament of the elbow, can avulse the medial epicondyle, and the apophyseal fragment could typically turn into lodged within the elbow joint. In children this can be tough to elicit, but typically a witness could also be obtainable. The two most necessary issues in the bodily examination are to doc neurovascular standing and to assess for elbow stability. Determination of stability contains determination of whether the elbow is dislocated, which could be assessed clinically and confirmed radiographically. Persistence of medial elbow stability may cause vital elbow disability in athletes or these doing heavy labor. Radiographs may affirm elevated displacement of the medial epicondylar fragment.
Buy retrovir 100mg with amex
Surgical treatment of displaced intraarticular fractures of the calcaneus: a combined lateral and medial approach. Open reduction and inside fixation of calcaneal fractures with a low profile titanium calcaneal perimeter plate. Osteosynthesis of displaced intraarticular fractures of the calcaneus: ends in 123 circumstances. The second metatarsal is recessed between the medial and lateral cuneiforms in the axial airplane and is positioned on the apex of the Roman arch within the coronal aircraft. The tarsometatarsal joints are stabilized by dorsal and plantar tarsometatarsal ligaments. Dorsal and plantar intermetatarsal ligaments provide further stability between the second by way of fifth metatarsal bases. The medial three tarsometatarsal joints and the adjoining intercuneiform and naviculocuneiform articulations (medial and center columns) have limited inherent motion, making these joints nonessential to normal foot operate and therefore comparatively expendable. The medial column refers to the first tarsometatarsal and navicular�medial cuneiform articulations; the center column consists of the second and third tarsometatarsal joints, and articulations between the navicular and middle and lateral cuneiforms, respectively. The fourth and fifth tarsometatarsal (lateral column) joints have distinctly extra inherent motion and are critical in lodging of the foot to uneven surfaces. These joints are considered important joints to regular foot perform and due to this fact nonexpendable. These accidents outcome from a mixture of axial load, and dorsiflexion, plantarflexion, abduction, or adduction (or variable combinations thereof) of the midfoot. The pathoanatomy is individually particular and extremely variable and will include a pure ligamentous harm, a pure bony damage (fracture), or a combination. While the harm classically contains the primary, second, and third tarsometatarsal joints, there could also be involvement of all five tarsometatarsal articulations, extension into the intercuneiform joints, or even fracture traces into the navicular or cuboid proximally, or metatarsal shafts or necks distally. In pure ligamentous patterns, the steadiness of the harm is dependent upon the standing of the plantar tarsometatarsal ligaments. Partial injuries (sprains) occur because of decrease energy and are extra widespread with axial load and plantarflexion, similar to in aggressive sports activities. In this instance, by definition the plantar tarsometatarsal ligaments remain intact, making the harm steady. When precisely identified, nonetheless, sufferers with these injuries can generally expect full restoration and return to activity with minimal long-term implications. A thorough examination of the involved foot and ankle additionally includes assessment of related accidents and any other areas of swelling or tenderness to palpation. Diffuse swelling of the midfoot or plantar ecchymosis on the midfoot suggests a Lisfranc injury. The physician should palpate the midfoot joints; pain at the midfoot with palpation suggests a Lisfranc harm (see Exam Table for Pelvis and Lower Extremity Trauma, pages 1 and 2). Anatomic specimen demonstrating the keystone of the Roman arch: the second metatarsal base is recessed between the medial and lateral cuneiforms (black arrow). The oblique view will reveal intra-articular displacement through the third, fourth, and fifth tarsometatarsal joints, and fractures of the third, fourth, and fifth metatarsal bases, lateral cuneiform, and cuboid. The doctor should check midfoot stability with passive flexion of the metatarsal heads and passive abduction and adduction through the forefoot. Pain at the tarsometatarsal joint region with passive forefoot vary of movement suggests a Lisfranc injury. Fluoroscopic stress views may be useful in more delicate accidents; however, these research are painful and customarily require anesthesia. Nonoperative therapy can be indicated for nondisplaced or minimally displaced extra-articular metatarsal base fractures with no intra-articular involvement (displacement) on weight-bearing radiographs. Because of the usually delicate nature of Lisfranc accidents and the negative penalties of misdiagnosis, if the findings are inconclusive, weight-bearing radiographs could also be repeated 2 to three weeks after the harm. Nonoperative administration consists of immobilization in a venous compression stocking and prefabricated fracture boot. The patient is allowed to bear weight to tolerance, and early development to vary of movement is encouraged. The patient continues within the fracture boot for 5 to 6 weeks, at which level upkeep of alignment or radiographic union is confirmed on repeat weight-bearing radiographs.
Generic retrovir 300 mg without prescription
The stab incisions (not shown) ought to be well distal to the pin�bone interface to stop soft tissue rigidity. An "advance�withdrawal" take a look at is carried out beneath stay fluoroscopy to confirm stability in addition to the extra-articular nature of the pins. The pin is advanced into the top, stopping several millimeters below the subchondral bone. I usually choose to place this pin beginning more proximally and anteriorly to the primary pin. If needed, a third pin can be added from the larger tuberosity downward into the shaft. This is helpful in small patients for higher buy in the head, however I usually avoid this pin because of a better fee of sentimental tissue complications. The shoulder is rotated and the information of the pins should seem to strategy the joint surface and then withdraw with continued rotation. In larger sufferers near or at skeletal maturity with adequate bone stock, cannulated screws could be inserted over a wire in the same style as described for threaded pins. I have discovered this method not often needed, nevertheless it does avoid the problem of pin administration (see below). With a sandbag or towel roll positioned between the shoulder blades, the patient is placed supine with the involved aspect close to the sting of the working desk. Intravenous anesthesia or acutely aware sedation could also be used, however I choose to perform the discount beneath common anesthesia, each for patient consolation and so I can proceed to open reduction if required. If unsuccessful, the clavicle can be grasped and pulled upward, especially in thin sufferers. Finally, the area may be prepared and draped and a towel clip used percutaneously to grasp the clavicle and reduce it. Gentle posterior pressure on the clavicle confirms the stability of the discount. The shoulder is taken by way of a range of motion and the reduction checked as properly. Finally, intraoperative fluoroscopy is used to confirm symmetry of the sternoclavicular joints. This allows careful publicity of the medial fracture (in the case of a true dislocation) or the physeal fracture site (in the case of a fracture-dislocation). The needle is handed by way of one drill gap, out across the fracture website, and up by way of the outlet in the corresponding fragment. After fixation, the reduction is tested for stability, and after confirmation of such, the wound is closed utilizing commonplace technique. Under the subcutaneous tissue lies the platysma muscle, which can also be break up according to the incision. The clavicle is exposed subperiosteally, starting laterally and dealing medially toward the joint. It is crucial to remain subperiosteal with the clip to avoid inadvertent damage to the vessels lying instantly posteriorly. For a pure dislocation, a figure 8 pattern through burr holes will safe the joint. Gapping at the fracture might signify interposed tissue, and the preparation should enable open publicity if required. The surgeon ought to keep away from putting the pins in the region of the axillary and musculocutaneous nerve. The skin must be dealt with carefully and multiple punctures averted to reduce delicate tissue issues. The surgeon ought to rigorously consider affected person age and remodeling capacity earlier than continuing with surgical procedure. The surgeon ought to settle for less-than-perfect discount in lieu of open reduction if potential to avoid the issues related to an open strategy. Sternoclavicular joint the surgeon ought to think about open discount and stabilization if doubt exists about stability. Closed reduction Open reduction Preoperative imaging can establish potential related injuries. Operative therapy often ends in passable therapeutic, although several reports observe a excessive fee of problems from operative therapy, including late fracture via a pin gap and late osteomyelitis. A battery-powered hand drill is helpful for securely greedy the pins and backing them out, as the information are threaded.
Diseases
- Juvenile hyaline fibromatosis
- Lymphoma, large-cell
- Hyperprolinemia type II
- Lambert Eaton syndrome
- Polycystic kidney disease, type 3
- 3-hydroxyacyl-coa dehydrogenase deficiency
- Fanconi syndrome, renal, with nephrocalcinosis and renal stones
- Stiff person syndrome
- Phosphate diabetes
Purchase retrovir 100 mg free shipping
Sensory examination should include, at minimal, mild contact sensation testing (or pin prick testing if necessary) of the autonomous zones of the radial, ulnar, and median nerves. Older youngsters may be able to adjust to formal two-point discrimination testing. Anatomically the shaft of the radius extends from probably the most proximal facet of the tubercle of Lister (which approximates the distal metaphyseal�diaphyseal junction) to the proximal base of the bicipital tuberosity. Classically, forearm shaft fractures are divided into distal third (pronator quadratus region), central third (pronator teres region), and proximal third (biceps and supinator region). Forward falls tend to contain a pronated forearm and backward falls a supinated forearm. Single-bone forearm shaft fractures ought to elevate vital suspicion regarding the presence of a Galeazzi or Monteggiatype damage (see Chap. Mechanisms of injury that involve little rotational force result in forearm fractures at practically the identical levels, while greater rotational pressure leads to fractures at somewhat different ranges. Spontaneous correction and enchancment of malaligned shaft fractures are thought of to occur in younger children through three mechanisms: Adjacent physes produce "straight bone" through regular growth. It has been mentioned that you need solely a thumb to check the motor function of all three major nerves: radial nerve extensor pollicis longus, ulnar nerve adductor pollicis, median nerve opponens pollicis. Peripheral nerves within the fractured extremity are assessed with the "rock-paper-scissors" methodology. The radial nerve (really the posterior interosseous nerve in the forearm) is examined with "paper"-extension of the fingers and wrist properly above a zero-degree wrist position. There is a threat of iatrogenic damage throughout surgical publicity of the proximal radial shaft. The ulnar nerve is examined with "scissors"-adducted thumb, abducted fingers, and flexor digitorum profundus perform to ring and pinky. This is the most typical iatrogenic nerve damage after inner fixation of forearm shaft fractures. The median is probably the most generally injured nerve after closed or open forearm shaft fractures. Flexion of the distal interphalangeal of the index finger and the interphalangeal of the thumb herald flexor digitorum profundus and flexor pollicis longus perform of those digits. Isolated palsy has been reported secondary to constrictive dressings and after proximal ulna fracture. Radius Ulna Level: Fracture degree has bearing on nonoperative versus operative decision making. Distal third Middle third Proximal third Pattern: Fracture pattern has bearing on nonoperative versus operative determination making. Bow (also often recognized as plastic deformation) Greenstick Complete Comminuted respect should be paid to the extent of the fractures when selecting a relatively neutral, pronated, or supinated forearm position. Initial above-elbow solid immobilization is the rule for all forearm shaft fractures, as this appropriately controls pronation�supination in addition to obeying the orthopaedic maxim of immobilizing the joints above and beneath the fracture. An additional good factor about above-elbow immobilization relates to the activity limitation it imposes; in some cases this will likely enhance the chances of maintaining a passable discount in an in any other case very lively buyer. Successful nonoperative treatment requires an eclectic mixture of anatomic data, skillful software of reduction methods, appreciation for transforming potential, and respect for the character of the delicate tissue envelope. Davis and Green reported a 10% lack of reduction price with greenstick fractures and a 25% fee with complete fractures. Apex volar greenstick fractures are thought of to characterize supination injuries that require a relative diploma of pronation to effect reduction. Apex dorsal greenstick fractures are thought of to be pronation accidents that require supination to assist reduction. Classic finger-trap and traction discount strategies are probably finest reserved for complete both-bone fracture patterns. When dealing with complete both-bone shaft fractures, Flexible intramedullary nail remedy of pediatric forearm shaft fractures focuses predominantly on displaced complete fractures, lots of which may have minor comminution (butterfly fragments usually lower than 25% of a shaft diameter). When full fractures occur in children youthful than about 8 to 10 years of age with angulation of at least 20 degrees within the distal third, 15 levels within the central third, or 10 degrees within the proximal third, risk�benefit discussions are applicable regarding additional efforts at fracture discount and attainable inside fixation.
Purchase retrovir 100mg with amex
This might represent buttonholing of the proximal fragment through the periosteum and brachialis muscle, making closed reduction tough. Approach the first factor to consider in determining the approach is the path of displacement of the distal fragment. In common, a transverse anterior incision via the antecubital fossa is essentially the most useful and cosmetic. If more visualization is required, this incision could be prolonged medially or laterally based on displacement, but this is rarely essential. Extension of the incision on the opposite facet of the displacement of the distal fragment permits for removing of soft tissue obstacles to discount. An inability to scale back the fracture may indicate that the proximal fragment has buttonholed via the brachialis muscle. Some surgeons have advocated a posterior strategy for severely comminuted fractures. Some newer articles have been published discovering no important increase in complication charges with delayed therapy. It is at this point that the neurovascular bundle ought to be positioned, if it has not but been recognized. This normally includes dissecting across the anterior side of the metaphyseal spike. Defining the outline of the distal fragment could be probably the most difficult aspect of the process. Reduction is obtained by reaching into the fracture web site with a hemostat and getting maintain of the reduce edge of the periosteum. This minimize edge is prolonged with scissors to enhance the size of the buttonhole and helps to release the distal fragment. The distal fragment is then brought anteriorly and reduced to the shaft fragment, which is maneuvered back by way of the buttonhole into its resting position posterior to the brachialis muscle. Alternatively, the surgeon can hold his or her thumb on the proximal fragment and push downward while an assistant applies traction to the forearm with the elbow flexed at 90 levels. Pinning Once a discount has been obtained, the fracture is fastened with clean Kirschner wires. Sagittal view of fracture with proximal fragment shown buttonholing though muscle and periosteum. Alternatively, a cross-pinning technique can be used with medial and lateral entry pins. Ideally, each the medial and lateral pins ought to cross proximal to the fracture website. The surgeon should make certain to have interaction both the medial and lateral columns of the distal fragment. The surgeon should broaden the buttonhole by way of the periosteum for better visualization. Pins ought to be maximally separated at the fracture site if three lateral pins are used. If medial and lateral pins are used, the surgeon should have interaction the medial and lateral columns of the distal fragment. A strip of Xeroform dressing could be wrapped across the pins, adopted by fluff dressings. Often a long-arm solid may be placed safely the subsequent day, with the arm flexed about eighty levels. This forged could be maintained till the pins are removed three or 4 weeks after surgical procedure. The affected person can then be positioned again into a sling and started on gentle range-of-motion workouts out of the sling for another 2 weeks. Families ought to be suggested about this longer interval of elbow stiffness in the instant postoperative interval. A 2001 study of 862 supracondylar fractures handled with open reduction found 55% excellent outcomes, 24% good results, 9% truthful results, and 12% poor results 5. Iatrogenic neurovascular damage Identification of neurovascular constructions is crucial.
Cheap 300mg retrovir free shipping
Often these fractures must be reduced in some equinus to enable for anatomic alignment and prevent recurvatum. Generally, metaphyseal distal tibial fractures which have failed closed management could be handled with cross-pinning using easy Kirschner wires. Large, medium, and even small external fixator sets could need to be out there depending on the dimensions of the kid. Syndesmosis accidents usually occur in the pediatric inhabitants solely at or near the time of skeletal maturity; thus, these injuries can usually be handled like grownup injuries. Untreated, the natural history of this syndrome involves a residual sensory deficit in the first dorsal internet house and contracture of the extensor hallucis longus and extensor digitorum brevis. Displaced fractures bear closed reduction under general anesthesia or acutely aware sedation, then casting for 3 to 6 weeks if displacement is successfully lowered to less than 2 mm. If still displaced greater than 4 mm, open reduction and inner fixation is undertaken. If displacement is 2 to 4 mm with less than 2 years of development remaining, casting is undertaken. Additionally, we observe up with patients with growth plate fractures at regular intervals till skeletal maturity. After preliminary fracture administration followup is maintained at 6-month intervals and will embody bilateral ankle radiographs. Cross-sectional view of the superior retinaculum tunnel, which may require launch with displaced physeal fractures. Patients presenting with severe ankle pain and tenderness, hypoesthesia or anesthesia in the first dorsal net house, weak spot of the extensor hallucis longus and extensor digitorum communis, and ache on passive stretch of the great toe could require launch of the superior extensor retinaculum. Extensor retinaculum syndrome of the ankle after harm to the distal tibial physis. Four weeks postoperatively the forged is modified to a weightbearing forged and the child is allowed to be weight bearing as tolerated for two or three extra weeks with a cast shoe. Occasionally adolescents may profit from bodily therapy for range of motion and proprioceptive conditioning. We advocate follow-up for no much less than 1 year, at 3, 6, and 12 months, then each 6 months till skeletal maturity for children with physeal injuries to monitor for untimely physeal closure. However, data for intra-articular triplane fractures have shown the significance of anatomic alignment of less than 2 mm of displacement after therapy. Ertl and coworkers3 demonstrated with a follow-up of 18 to 36 months that "residual displacement of two millimeters or extra after discount was related to a less than optimum end result until the epiphyseal fracture was outdoors the first weight-bearing area of the ankle. Reflex sympathetic dystrophy or complex regional pain syndrome is a continual pain syndrome that can develop after these ankle accidents. It is characterized by ache out of proportion that persists past a typical recovery timeframe and may also entail swelling, skin colour changes, and limited range of movement. Treatment can embody medicines, therapy, psychological counseling, and sympathetic nerve blocks; in extreme instances sympathectomy or implantation of a dorsal column stimulator has been proposed. Superior extensor retinaculum syndrome, as described above, can result in residual numbness within the great toe web space and protracted pain and weak spot within the toe extensors. Malunion of fractures can occur with operative or nonoperative therapy or could be a secondary consequence of premature physeal closure. Osteochondral injury in ankle fractures can in the end result in symptomatic posttraumatic osteoarthritis, and research have demonstrated that anatomic reduction is necessary to prevent this complication. If vital chondral injury does occur in the younger patient population, drilling for focal posttraumatic osteochondritis dissecans lesions may be profitable. In extreme circumstances with osteochondral damage, osteochondral allografting may be tried. Casts applied too tightly or not appropriately split can result in acute compartment syndrome. Osteochondritis Dissecans of the Capitellum this time period is used to describe the condition of compromised subchondral bone within the capitellum of adolescents, which might lead to secondary articular floor separation. Synovitis: occasional gentle palpable effusion Later levels: Patients complain of mechanical symptoms, including locking and catching and limited flexion and extension; palpable synovial thickening and an effusion may also be discovered. The ulnohumeral joint is a hinge joint that allows for flexion and extension of the elbow, whereas the radiocapitellar and radioulnar joints are trochoid joints that permit for axial rotation and pivoting of the elbow. The capitellum articulates with the rim of the radial head throughout flexion�extension and pronation�supination.
Retrovir 100 mg otc
Generally, when the tibia could be easily shifted anteriorly, the tibia is reduce first, but if the knee is tight or good exposure is tough to get hold of on the tibial plateau, the femoral condyles are the first to be cut. Most newer femoral cutting blocks provide slots for performing distal, anterior, posterior, and chamfer cuts by utilizing a single block, thereby decreasing the time. Necessary adjustments have to be made to make the guide align with the middle of the interspinous eminence of the plateau, the tibial shaft, and the middle of the ankle mortis, which is, actually, three to 5 mm medial to the intermalleolar axis. By sliding the distal finish of the guide mediolaterally at the ankle, a final adjustment can be made to centralize it over the middle of the talus and to minimize the chance of varus inclination of the cut. Set the proximal half to get hold of three to 5 degrees of posterior slope in the sagittal plane. Bear in thoughts that jig methods fitted to the anterior floor of the proximal tibia will generally tend to align in excessive inside rotation due to the everted patellar tendon. Fit the proximal cutting block snugly up in opposition to the tibial cortex to enhance the accuracy of the resection. This minimize should be made at right angles to the anatomic axis of the tibia in the coronal plane. The bone resected ought to have approximately the identical thickness as the ultimate tibial element, including the metal base plate and polyethylene liner. To shield the posterior neurovascular bundle, stop cutting the earlier couple of millimeters of bone by noticed and crack the remaining afterward by levering or utilizing an osteotome. Establish the anatomic boundary of the tibial metaphysis by removing the osteophytes. The strap of the distal finish of the extramedullary alignment guide is hooked up above the ankle, tunings are accomplished, and the proximal finish is pinned to the higher tibial metaphysis. Touching the anterior surface of the femoral shaft with the opposite hand can be a good guide to the direction of drilling. It is essential to stop the noticed blade from bending or going ahead in an undesired course whereas continuing by way of the osteotomy line, significantly throughout resection of exhausting and sclerotic bone. The amount of bone to be resected must be exactly equal to the thickness of the ultimate femoral element. Maximally flex the knee to cut back the chance of damage to the posterior neurovascular bundle during posterior sawing. Anterior and Posterior Chamfer Cuts Anterior and posterior chamfer cuts are important for the prosthesis to match over the distal femur. Anterior and Posterior Femoral Condyle Cuts Patellar Preparation Making accurate cuts is crucial to obtain proper measurement and rotation of the ultimate femoral part. External rotation means counterclockwise rotation for the best knee and clockwise rotation for the left knee. In knees with out deformity, external rotation usually leads to removing of more bone from the medial posterior condyle. Erosion of the posterior femoral condyles can distort this posterior condylar axis. To obtain an actual measurement of the patellar thickness, the prepatellar bursa ought to be dissected to utterly expose the anterior floor of the patella. Femoral part rotation is determined by reference lines used for performing the distal femoral reduce. An osteotome is used to free small remnant portions of uncut bone and removing posterior osteophytes. Calipers are used to assess the patellar thickness before the retropatellar osteotomy. In knees with advanced or extreme deformity, however, cautious stepwise launch is important. Insert the trial elements and check the steadiness of the knee after each step of the process. When the deformity is extreme and results in lack of the integrity of the ligaments, be ready for utility of a constrained prosthesis. To obtain a correct soft tissue balance, initially remove the offending osteophytes until the anatomic margins of the bone are decided. Correction of Valgus Deformity Correction of Flexion Contracture Use a curved osteotome to release osteophytes behind the femur and then extract them with a rongeur. Strip the adherent capsule from the posterior facet of the femur to reestablish the unique recess. In knees with preoperative moderate to extreme flexion contracture, it additionally is important to minimize the posterior capsule transversely and to launch the tendinous origins of the gastrocnemius.