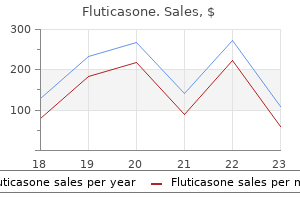
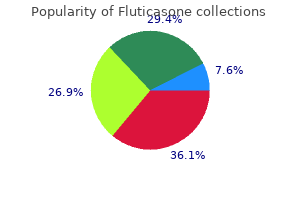
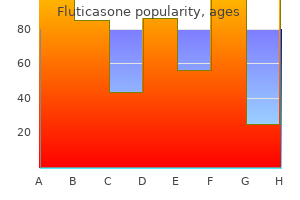
Fluticasone dosages: 500 mcg, 250 mcg, 100 mcg
Fluticasone packs: 1 inhalers, 2 inhalers, 3 inhalers, 4 inhalers, 5 inhalers

Buy fluticasone with paypal
Calcaneus (C) Calcaneal spur (arrow) Bursa (not seen in radiograph) C Sural Nerve Grafts Pieces of the sural nerve are sometimes used for nerve grafts in procedures similar to repairing nerve defects resulting from wounds. In skinny individuals, these branches can usually be seen or felt as ridges beneath the skin when the foot is plantarflexed. Injections of an anesthetic agent round these branches in the ankle region, anterior to the palpable portion of the fibula, anesthetizes the skin on the dorsum of the foot (except the web between and adjoining surfaces of the first and 2nd toes) extra broadly and successfully than extra local injections on the dorsum of the foot for superficial surgical procedure. A diminished or absent dorsalis pedis pulse usually suggests vascular insufficiency ensuing from arterial disease. The five P signs of acute arterial occlusion are ache, pallor, paresthesia, paralysis, and pulselessness. In these cases, the dorsalis pedis artery is replaced by an enlarged perforating fibular artery. Hemorrhaging Wounds of Sole of Foot Puncture wounds of the only real of the foot involving the deep plantar arch and its branches usually result in extreme bleeding, usually from each ends of the minimize artery due to the ample anastomoses. Medial plantar nerve compression may occur during repetitive eversion of the foot. Infections on the lateral facet of the foot initially produce enlargement of popliteal lymph nodes (popliteal lymphadenopathy); later, the inguinal lymph nodes could enlarge. Palpation of Dorsalis Pedis Pulse the dorsalis pedis artery pulse is evaluated throughout a physical examination of the peripheral vascular system. � There is similarity to the arrangement of muscle tissue in the palm of the hand, however the muscle tissue of the foot typically reply as a group somewhat than individually, appearing to keep the longitudinal arch of the foot or push a portion of it tougher in opposition to the bottom to maintain balance. � the movements of abduction and adduction produced by the interossei are toward or away from the 2nd digit. � the foot has two intrinsic muscles on its dorsum that increase the long extensor muscular tissues. � these muscles are particularly lively in fixing the medial forefoot for the propulsive push off. � the skin of the medial and lateral sides of the foot is innervated by the saphenous and sural nerves, respectively. � the plantar aspect of the foot receives innervation from the larger medial and smaller lateral plantar nerves. � the medial plantar nerve supplies extra skin (the plantar facet of the medial three and half toes and adjacent sole) however fewer muscles (the medial hallux and 1st lumbrical muscles only) than the lateral plantar nerve. Arteries of foot: the dorsal and plantar arteries of the foot are terminal branches of the anterior and posterior tibial arteries, respectively. It additionally contributes to formation of the deep plantar arch by way of its terminal deep plantar artery. � the smaller medial and larger lateral plantar arteries supply the plantar side of the foot, the latter working in vascular planes between the first and 2nd layers after which, because the plantar arch, the third and 4th layers of the intrinsic muscles. � Except for the scarcity of a superficial plantar arch, the arterial pattern of the foot is similar to that of the hand. � Lymph from the lateral foot follows the small saphenous vein and drains initially to the popliteal lymph nodes and then by deep lymphatic vessels to the deep inguinal nodes. The heavy, distinguished acetabular rim of the acetabulum consists of a semilunar articular part lined with articular cartilage, the lunate floor of the acetabulum (text continues on p. The decrease limb joints are (A) those of the pelvic girdle connecting the free decrease limb to the vertebral column, (B) the knee and tibiofibular joint, and (C) tibiofibular syndesmosis, ankle joint, and the many joints of the foot. The joint was disarticulated by cutting the ligament of the pinnacle of the femur and retracting the head from the acetabulum. Relative strengths are indicated by arrow width: Anteriorly, the muscles are much less plentiful but the ligaments are robust; posteriorly, the muscular tissues predominate. In this coronal section of hip joint, the acetabular labrum and transverse acetabular ligament, spanning the acetabular notch (and included within the plane of section here), extend the acetabular rim in order that a whole socket is formed. The angle of Wiberg (see text) is used radiographically to decide the diploma to which the acetabulum overhangs the head of the femur. Several completely different strains and curvatures are used within the detection of hip abnormalities (dislocations, fractures, or slipped epiphyses). A fossa that crosses the road suggests an acetabular fracture with inward displacement.
Diseases
- Dentatorubral-pallidoluysian atrophy
- Hereditary paroxysmal cerebral ataxia
- Combarros Calleja Leno syndrome
- Vernal keratoconjunctivitis
- Kostmann syndrome
- Tibiae bowed radial anomalies osteopenia fracture
Generic 500 mcg fluticasone amex
The superior mesenteric artery, through its branch, the inferior pancreaticoduodenal artery, supplies the duodenum distal to the entry of the bile duct. The basis of this transition in blood provide is embryological; this is the junction of the foregut and midgut. The posterior lymphatic vessels pass posterior to the top of the pancreas and drain into the superior mesenteric lymph nodes. The nerves of the duodenum derive from the vagus and greater and lesser (abdominopelvic) splanchnic nerves by means of the celiac and superior mesenteric plexuses. The nerves are subsequent conveyed to the duodenum by way of peri-arterial plexuses extending to the pancreaticoduodenal arteries (see additionally "Summary of the Innervation of the Abdominal Viscera," p. The terminal ileum often lies in the pelvis from which it ascends, ending within the medial side of the cecum. Between the 2 layers of the mesentery are the superior mesenteric vessels, lymph nodes, a variable amount of fat, and autonomic nerves. The ileocolic and proper colic arteries on the proper side and the left colic and sigmoid arteries on the left side originally coursed within mesenteries (ascending and descending mesocolons) that later fused to the posterior wall; they are often re-established surgically. The sympathetic fibers in the nerves to the jejunum and ileum originate in the T8�T10 segments of the spinal wire and attain the superior mesenteric nerve plexus through the sympathetic trunks and thoracic abdominopelvic (greater, lesser, and least) splanchnic nerves. The presynaptic sympathetic fibers synapse on cell bodies of postsynaptic sympathetic neurons in the celiac and superior mesenteric (prevertebral) ganglia. Specialized lymphatic vessels in the intestinal villi (tiny projections of the mucous membrane) that take in fat are known as lacteals. They empty their milk-like fluid into the lymphatic plexuses in the partitions of the jejunum and ileum. The lacteals drain in turn into lymphatic vessels between the layers of the mesentery. The massive intestine could be distinguished from the small gut by: � Omental appendices: small, fatty, omentum-like projections. The teniae coli (thickened bands of easy muscle representing a lot of the longitudinal coat) start at the base of the appendix as the thick longitudinal layer of the appendix separates into three bands. To study the colon, a barium enema has been given after the bowel is cleared of fecal materials by a cleansing enema. Single contrast barium research demonstrate the semilunar folds demarcating the haustra. Following the only distinction examine, the affected person has evacuated the barium and the colon was distended with air for this double-contrast examine. The frenulum is a fold (more evident in cadavers) that runs from the ileocecal valve alongside the wall at the junction of the cecum and ascending colon. The approximate incidences of assorted places of the appendix, based mostly on an analysis of 10,000 circumstances, are shown. It was believed that when the cecum is distended or when it contracts, the lips and frenula actively tighten, closing the valve to prevent reflux from the cecum into the ileum. The sympathetic nerve fibers originate within the decrease thoracic part of the spinal twine, and the parasympathetic nerve fibers derive from the vagus nerves. It passes superiorly on the right side of the stomach cavity from the cecum to the best lobe of the liver, where it turns to the left on the right colic flexure (hepatic flexure). This flexure lies deep to the 9th and tenth ribs and is overlapped by the inferior part of the liver. The ascending colon is narrower than the cecum and is secondarily retroperitoneal alongside the best facet of the posterior stomach wall. The ascending colon is separated from the anterolateral belly wall by the greater omentum. This artery parallels and extends the length of the colon near its mesenteric border. It crosses the stomach from the proper colic flexure to the left colic flexure, where it turns inferiorly to turn out to be the descending colon.
Purchase fluticasone australia
� It is encircled by voluntary muscle of the inferior part of the exterior urethral sphincter before perforating the perineal membrane. � the intermediate and spongy parts of the urethra are provided and drained by the identical dorsal (blood) vessels of the penis, however differ in terms of innervation and lymphatic drainage. Scrotum: the scrotum is a dynamic, fibromuscular cutaneous sac for the testes and epididymides. � the erectile bodies are bound together by deep fascia of the penis, except on the root the place they separate into the crura and bulb of the penis. � the crura attach to the ischiopubic rami, but all parts of the basis are connected to the perineal membrane. � At the junction of the root and body, the penis is hooked up to the pubic symphysis by the suspensory ligament of the penis. � the glans penis is a distal expansion of the corpus spongiosum, which has the exterior urethral orifice at its tip and a projecting corona that overhangs the neck of the glans. The terminal helicine arteries open to engorge the sinuses with blood at arterial pressure, inflicting penile erection. � In addition, the bulbospongiosus muscle constricts the bulb of the penis to categorical the final drops of urine or semen. The vulva serves: � As sensory and erectile tissue for sexual arousal and intercourse. Moisture usually retains the labia minora passively apposed, keeping the vestibule of vagina closed (B) until spread apart as in (C). The labia majora are thicker anteriorly the place they join to form the anterior commissure. Posteriorly, in nulliparous women (those never having borne children), they merge to form a ridge, the posterior commissure, which overlies the perineal body and is the posterior limit of the vulva. Skin, subcutaneous tissue (including perineal fascia and ischio-anal fats bodies), and the investing fascia of the muscle tissue have been removed. Deeper dissection of the superficial pouch (right side) reveals the bulbs of the vestibule and the higher vestibular glands. Superficial transverse perineal muscle Deep Perineal Superficial nerve Posterior labial nerve and artery * Perineal nerve Ischial tuberosity Levator ani muscle * Perineal body 430 Chapter three � Pelvis and Perineum openings of the ducts of the para-urethral glands. The larger vestibular glands are spherical or oval and are partly overlapped posteriorly by the bulbs of the vestibule. The inside pudendal artery supplies most of the skin, external genitalia, and perineal muscle tissue. The labial veins are tributaries of the internal pudendal veins and accompanying veins of the internal pudendal artery. Venous engorgement during the pleasure part of the sexual response causes a rise within the dimension and consistency of the clitoris and the bulbs of the vestibule of the vagina. Although the interior surface of each labium minus consists of skinny moist skin, it has the pink shade typical of mucous membrane and accommodates many sebaceous glands and sensory nerve endings. Together, the physique and glans clitoris are approximately 2 cm in length and <1 cm in diameter. The glans clitoris is probably the most extremely innervated a half of the clitoris and is densely equipped with sensory endings. The exterior urethral orifice is situated 2�3 cm postero-inferior to the glans clitoris and anterior to the vaginal orifice. The surrounding soft tissues have been removed to reveal the elements of the clitoris. In this view, the pores and skin, subcutaneous tissue, and ischio-anal fat our bodies have been eliminated. The anterior side of the vulva (mons pubis, anterior labia) is equipped by derivatives of the lumbar plexus: the anterior labial nerves, derived from the ilio-inguinal nerve, and the genital department of the genitofemoral nerve. Deep and muscular branches of the perineal nerve supply the orifice of the vagina and superficial perineal muscle tissue. The operation carried out throughout childhood removes the prepuce of the clitoris and generally also removes half or all of the clitoris and labia minora. This disfiguring procedure is erroneously thought to inhibit sexual arousal and gratification. Vulvar Trauma the extremely vascular bulbs of the vestibule are vulnerable to disruption of vessels as the outcome of trauma.
Order fluticasone 250 mcg with amex
This uncommon cervical canal outcomes from persistence of remnants of the 2nd pharyngeal pouch and 2nd pharyngeal groove (Moore et al. Branchial Sinuses and Cysts When the embryonic cervical sinus fails to disappear, it could retain its reference to the lateral surface of the neck by a branchial sinus, a slender canal. Esophageal Injuries Esophageal injuries are the rarest sorts of penetrating neck trauma; nevertheless, they cause most issues after a surgical procedure or different therapy. Structures in danger are the cervical pleurae, apices of lungs, thyroid and parathyroid glands, trachea, esophagus, widespread carotid arteries, jugular veins, and the cervical area of the vertebral column. Structures in danger are the superior poles of the thyroid gland, thyroid and cricoid cartilages, larynx, laryngopharynx, carotid arteries, jugular 1050 Chapter eight � Neck veins, esophagus, and cervical region of the vertebral column. � Typically, the thyroid gland is roughly H-shaped, with proper and left lobes linked by a thin central isthmus. � Typically, there are 4 parathyroid glands (two superior and two inferior) inside the capsule of the thyroid gland or in the gland itself. � Superior thyroid veins accompany the arteries of the identical name, draining the area they supply. � the larynx additionally modifies the exit of air from the tract to produce tone for vocalization. � All the laryngeal muscular tissues besides one (posterior crico-arytenoid) take part in closure of the rima glottidis. � Otherwise, opening occurs passively by the tidal flow of air, with the opposite muscles controlling the quantity and nature of resistance offered at the rima glottidis to produce tone and control its pitch. � the recurrent laryngeal nerve (via its terminal department, the inferior laryngeal nerve) is the motor nerve, which provides all muscles of the larynx, with one exception. � the superior, noncollapsible nasopharynx is solely respiratory, and the air and food pathways cross inside the oropharynx and laryngopharynx. � the contractile pharynx is exclusive inside the alimentary tract in being constructed of voluntary muscle with the round layer (pharyngeal constrictors) external to longitudinal muscle, the stylopharyngeus, palatopharyngeus, and salpingopharyngeus. � the flat posterior wall of the pharynx, abutting the musculoskeletal neck at the retropharyngeal house, is without openings; nevertheless, its anterior wall includes openings to the nostril, mouth, and larynx. � the soft palate serves as a flap valve regulating access to or from the nasopharynx and oropharynx, whereas the larynx is the "valve" ultimately separating meals and air earlier than they enter the esophagus and trachea, respectively. � the superior two openings of the pharynx, which hook up with the external environment, are encircled by a hoop of lymphoid (tonsillar) tissue. � Innervation of the pharynx is from the pharyngeal nerve plexus, with the vagus offering the motor fibers and the glossopharyngeal offering sensory fibers. � Immediately inferior, because the outer muscular layer turns into longitudinal, the esophagus begins. � Also at roughly this point, sensory and motor innervation is transferred to the recurrent laryngeal nerves. This overview demonstrates the course of the thoracic duct and web site of the termination of the thoracic and right lymphatic ducts. Other deep cervical nodes include the prelaryngeal, pretracheal, paratracheal, and retropharyngeal nodes. Often, however, these lymphatic trunks enter the venous system independently within the area of the best venous angle. During the process, the deep cervical lymph nodes and tissues around them are eliminated as completely as possible. The goal of the dissection is to take away all tissue that bears lymph nodes in one piece. Injuries to Vestibulocochlear Nerve; Deafness; Acoustic Neuroma; Trauma and Vertigo. These embody particular sensory fibers conveying style and scent (special visceral afferent fibers) and people serving the particular senses of vision, listening to, and balance (special somatic afferent fibers). They are referred to as cranial nerves because they emerge through foramina or fissures within the skull and are coated by tubular sheaths derived from the cranial meninges. On the premise of the embryologic/phylogenetic derivation of certain muscles of the top and neck,1 some motor fibers conveyed by cranial nerves to striated muscle have historically been categorized as "special visceral. The basal surfaces of the bipolar olfactory receptor neurons of the nasal cavity of 1 facet give rise to central processes which might be collected into approximately 20 olfactory nerves (L. Historically, the sternocleidomastoid and trapezius have been categorised as branchiomeric muscles; college students might even see them categorized as such in different references.
Bai Guo Ye (Ginkgo). Fluticasone.
- What other names is Ginkgo known by?
- Are there safety concerns?
- Improving thinking in young people.
- Coughs, asthma, bronchitis, urinary problems, cognitive problems related to Lyme disease, digestion disorders, chronic fatigue syndrome (CFS), scabies, and skin sores when the seeds are used.
- Are there any interactions with medications?
- Sexual problems related to antidepressant medicines.
- Sexual problems in women.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96352
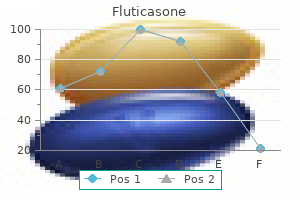
Discount 250mcg fluticasone visa
The tricuspid and truncal valves, by contrast, are normally discontinuous, separated by the ventriculoinfundibular fold. Rarely, the mitral, tricuspid, and truncal valves could all be in continuity, or, much more not often, they might lack continuity altogether. The origins and proximal courses of the coronary arteries are highly variable and have an increased incidence of a single coronary artery origin. Approximately one-third of sufferers with truncus arteriosus have a right-sided aortic arch. Unilateral absence of a pulmonary artery might happen in as a lot as 16% of patients and usually happens on the aspect of the aortic arch. This is in contradistinction to tetralogy of Fallot, by which absence of the pulmonary artery happens on the alternative side of the aortic arch. In one sequence, 10% of patients with truncus arteriosus had interruption of the aortic arch. Other associated anomalies include aortic arch hypoplasia, aortic coarctation, persistent left superior vena cava, aberrant right subclavian artery from the descending thoracic aorta, and atrial septal defects (especially secundum type). How to Approach the Image Radiographic features of truncus arteriosus depend on the amount of pulmonary blood flow and pulmonary resistance. Patients with truncus arteriosus with unrestricted blood circulate to the lungs present with pulmonary overcirculation and heart failure. In distinction, patients with truncus arteriosus with pulmonic stenosis show pulmonary undercirculation. Chest radiograph of a 2-day-old boy with kind 1 truncus arteriosus and interruption of the aortic arch who presented with a murmur on the left lower sternal border. There is cardiomegaly with rounding and upward rotation of the cardiac apex suggestive of proper ventricular enlargement. Pulmonary vascular redistribution and indistinctness of the pulmonary vessels are consistent with reasonable congestive coronary heart failure. The presence of a right aortic arch and pulmonary overcirculation should alert the radiologist to the potential for truncus arteriosus. Cross-sectional imaging can clearly reveal irregular truncal valvular morphology and the relationship of the truncal valve to the interventricular septum. Postoperative cross-sectional imaging could additionally be helpful for anatomic and functional problem solving. Type I: the main pulmonary artery is a branch of the common trunk and provides rise to proper and left pulmonary arteries. A mixed sort of truncus arteriosus happens with unilateral absence of a pulmonary artery. Complete primary surgical repair is carried out within the neonatal period to prevent pulmonary vascular obstructive illness brought on by elevated strain in the pulmonary arteries. Moderate to severe truncal valve insufficiency before restore and interruption of the aortic arch are conditions related to decreased postoperative survival. Conduit substitute or revision is almost all the time needed after full restore of truncus arteriosus with a median time to reoperation of 5 to 6 years. For patients with truncal valve insufficiency before complete repair, truncal valvuloplasty method could also be carried out. The proximal proper subclavian artery (arrow) is occluded with distal reconstitution by way of the proper vertebral artery (dotted arrow). Key Points In truncus arteriosus, a single arterial trunk arises from a single semilunar valve at the base of the heart, which gives rise to the systemic, coronary, and pulmonary arteries. All forms of truncus arteriosus could additionally be sophisticated by ostial or department pulmonary arterial stenosis or elevated pulmonary vascular resistance, leading to cyanosis. Truncal valve insufficiency is considered one of the most common complications and will present concurrently with pulmonary arterial stenosis. If truncal valve insufficiency is severe, heart failure shall be present shortly after birth. Late follow-up of 1095 patients undergoing operation for complex congenital heart illness utilizing pulmonary ventricle to pulmonary artery conduits.
Buy fluticasone 250 mcg low price
� the contents of the spermatic twine are the ductus deferens and neurovascular constructions, which trailed the testis as it relocated from the posterior stomach wall throughout growth. Scrotum: the scrotum is the integumentary sac shaped from the labioscrotal swellings of the male to home the testes after their relocation. � the scrotum receives anterior scrotal arteries from the thigh (via the external pudendal artery), posterior scrotal arteries from the perineum (internal pudendal artery), and internally cremasteric arteries from the abdomen (inferior epigastric artery). � Each testis is engulfed, except posteriorly and superiorly, by a double-layered serous sac, the tunica vaginalis, derived from the peritoneum. � the outer surface of the testis is roofed with the fibrous tunica albuginea, which is thickened internally and posteriorly as the mediastinum of the testis from which septa radiate. The tubules converge and empty into the rete testis within the mediastinum, which is linked in flip to the epididymis by the efferent ductules. � the innervation, blood vasculature, and lymphatic drainage all replicate the posterior belly origin of the testes and are, for the primary half, independent of the surrounding scrotal sac. � the epididymis is formed by the highly convoluted and compacted duct of the epididymis leading from the efferent ductules to the ductus deferens. Both layers of peritoneum consist of mesothelium, a layer of easy squamous epithelial cells. The parietal peritoneum is served by the same blood and lymphatic vasculature and the same somatic nerve supply, as is the region of the wall it strains. Pain from the parietal peritoneum is usually nicely localized, apart from that on the inferior floor of the central part of the diaphragm, where innervation is supplied by the phrenic nerves (discussed later on this chapter); irritation right here is commonly referred to the C3�C5 dermatomes over the shoulder. The visceral peritoneum and the organs it covers are served by the identical blood and lymphatic vasculature and visceral nerve supply. Consequently, ache from foregut derivatives is normally experienced within the epigastric region, that from midgut derivatives within the umbilical region, and that from hindgut derivatives within the pubic region. Retroperitoneal organs such because the kidneys are between the parietal peritoneum and the posterior stomach wall and have parietal peritoneum solely on their anterior surfaces (often with a variable quantity of intervening fat). The peritoneal cavity is within the abdominal cavity and continues inferiorly into the pelvic cavity. The peritoneal cavity is a possible area of capillary thinness between the parietal and visceral layers of peritoneum. These viscera are linked to the belly wall by a mesentery of variable size, which consists of two layers of peritoneum with a thin layer of loose connective tissue between them. Generally, viscera that change relatively little in dimension and shape, such as the kidneys, are retroperitoneal, whereas viscera that undergo marked adjustments in shape owing to filling, emptying, and peristalsis, such because the stomach, are invested with visceral peritoneum. As organs protrude into the peritoneal sac, their vessels, nerves, and lymphatics stay related to their extraperitoneal (usually retroperitoneal) sources or locations in order that these connecting structures lie between the layers of the peritoneum forming their mesenteries. Initially, the whole primordial gut is suspended within the heart of the peritoneal cavity by a posterior mesentery attached to the midline of the posterior physique wall. Lymphatic vessels, significantly on the inferior floor of the constantly active diaphragm, take in the peritoneal fluid. This progress (and later, the activity of the gut) is accommodated by the development of a serous cavity inside the trunk that houses the increasingly lengthy and convoluted intestine in a comparatively compact area. Early in its growth, the embryonic body cavity (intraembryonic coelom) is lined with mesoderm, the primordium of the peritoneum. For instance, throughout development, the rising coiled mass of small gut pushes the part of the intestine that can turn out to be the descending colon to the left aspect and presses its mesentery against the posterior abdominal wall. As a end result, the colon turns into fixed to the posterior stomach wall on the left facet with peritoneum masking solely its anterior aspect. Thus, the descending colon of the adult can be freed from the posterior body wall (surgically mobilized) by incising the peritoneum along the lateral border of the descending colon and then bluntly dissecting alongside the aircraft of the fusion fascia, elevating the neurovascular constructions from the posterior body wall till the midline is reached. Several components of the gastrointestinal tract and related organs turn out to be secondarily retroperitoneal. After descending, it folds again and attaches to the anterior surface of the transverse colon and its mesentery. A peritoneal ligament consists of a double layer of peritoneum that connects an organ with one other organ or to the stomach wall. The hepatogastric and hepatoduodenal ligaments are steady elements of the lesser omentum and are separated only for descriptive comfort. The abdomen is linked to the: � Inferior surface of the diaphragm by the gastrophrenic ligament.
Purchase 250mcg fluticasone with visa
Such deviation occurs particularly in females, and its frequency increases with age. Often hard corns (inflamed areas of thick skin) also type over the proximal interphalangeal joints, especially of the little toe. Pes Planus (Flatfeet) the flat appearance of the only of the foot before age three is normal; it results from the thick subcutaneous fat pad within the sole. The extra widespread flexible flatfeet outcome from unfastened or degenerated intrinsic ligaments (inadequate passive arch support). Flexible flatfeet is frequent in childhood however normally resolves with age as the ligaments develop and mature. Acquired flatfeet ("fallen arches") are likely to be secondary to dysfunction of the tibialis posterior (dynamic arch support) owing to trauma, degeneration with age, or denervation. Flatfeet are common in older people, significantly if they undertake much unaccustomed standing or acquire weight rapidly, including stress on the muscle tissue and growing the strain on the ligaments supporting the arches. � Compensation is attempted by several features, including (1) strong intrinsic, extracapsular, and intracapsular ligaments; (2) splinting by many surrounding tendons (including the iliotibial tract); and (3) menisci that fill the spatial void, offering mobile articular surfaces. Tibiofibular joints: the tibiofibular joints include a proximal synovial joint, an interosseous membrane, and a distal tibiofibular syndesmosis, consisting of anterior, interosseous, and posterior tibiofibular ligaments. Ankle joint: the ankle (talocrural) joint is composed of a superior mortise, fashioned by the weight-bearing inferior surface of the tibia and the two malleoli, which receive the trochlea of the talus. � Injury occurs primarily by inadvertent inversion of the plantarflexed, weight-bearing foot. Joints of foot: Functionally, there are three compound joints in the foot: (1) the clinical subtalar joint between the talus and the calcaneus, the place inversion and eversion occur about an indirect axis; (2) the transverse tarsal joint, where the midfoot and forefoot rotate as a unit on the hindfoot round a longitudinal axis, augmenting inversion and eversion; and (3) the remaining joints of the foot, which permit the pedal platform (foot) to kind dynamic longitudinal and transverse arches. It extends between and connects the shoulder and the elbow, and consists of anterior and posterior areas of the arm, centered across the humerus. These characteristics are especially marked within the hand when performing manual actions, such as buttoning a shirt. Synchronized interplay happens between the joints of the upper limb to coordinate the intervening segments to perform smooth, environment friendly motion on the most workable distance or position required for a particular task. Efficiency of hand function results in massive part from the power to place it in the correct place by movements at the scapulothoracic, glenohumeral, elbow, radio-ulnar, and wrist joints. Shoulder: proximal segment of the limb that overlaps elements of the trunk (thorax and back) and decrease lateral neck. The pelvic girdle consists of the two hip bones linked to the sacrum (see Chapter 5). Both girdles possess a big flat bone located posteriorly, which provides for attachment of proximal muscular tissues, and connects with its contralateral companion anteriorly via small bony braces, the pubic rami and clavicles. However, the flat iliac bones of the pelvic girdle are additionally connected posteriorly by way of their main attachment to the sacrum through the essentially rigid, weight-transferring sacro-iliac joints. This posterior connection to the axial skeleton locations the lower limbs inferior to the trunk, enabling them to be supportive as they function primarily in relation to the line of gravity. Furthermore, as a outcome of the 2 sides are connected each anteriorly and posteriorly, the pelvic girdle varieties a whole inflexible ring that limits mobility, making the actions of 1 limb markedly affect the actions of the opposite. Thus, the movement of 1 higher limb is unbiased of the opposite, and the limbs are able to function successfully anterior to the physique, at a distance and degree that enable precise eye�hand coordination. In each the upper and the lower limbs, the lengthy bone of essentially the most proximal section is the largest and is unpaired. Although the paired bones of both the leg and forearm flex and lengthen as a unit, only these of the upper limb are able to transfer (supinate and pronate) relative to each other; the bones of the leg are mounted in the pronated place. The digits of the upper limb (fingers together with the thumb) are essentially the most mobile components of either limb. The clavicle: � Serves as a moveable, crane-like strut (rigid support) from which the scapula and free limb are suspended, maintaining them away from the trunk so that the limb has maximum freedom of movement. The strut is movable and permits the scapula to move on the thoracic wall on the "scapulothoracic joint,"1 growing the vary of motion of the limb. The bone acts as a mobile strut (supporting brace) connecting the upper limb to the trunk; its size allows the limb to pivot around the trunk. Although designated as a protracted bone, the clavicle has no medullary (marrow) cavity. The superior floor of the clavicle, lying just deep to the pores and skin and platysma (G.
Cheap fluticasone generic
The bones of the elbow area, demonstrating the connection of the distal humerus and proximal ulna and radius throughout extension of the elbow joint. The relationship of the humerus and forearm bones throughout flexion of the elbow joint. For articulation with the humerus, the ulna has two outstanding projections: (1) the olecranon, which projects proximally from its posterior facet (forming the purpose of the elbow), and serves as a short lever for extension of the elbow, and (2) the coronoid process, which initiatives anteriorly. The articulation between the ulna and humerus primarily allows solely flexion and extension of the elbow joint, although a small amount of abduction� adduction occurs during pronation and supination of the forearm. On the lateral side of the coronoid process is a clean, rounded concavity, the radial notch, which receives the broad periphery of the head of the radius. Between it and the distal part of the coronoid process is a concavity, the supinator fossa. The deep a part of the supinator muscle attaches to the supinator crest and fossa (6. Proximally, the smooth superior aspect of the discoid head of the radius is concave for articulation with the capitulum of the humerus throughout flexion and extension of the elbow joint. Its lateral aspect becomes increasingly ridge-like, terminating distally in the radial styloid course of. The distal epiphysis of the ulna has ossified, however all of the epiphyseal plates (lines) remain open. Augmenting movement at the wrist joint, the two rows of carpal bones glide on one another; in addition, every bone glides on those adjacent to it. The proximal bases of the metacarpals articulate with the carpal bones, and the distal heads of the metacarpals articulate with the proximal phalanges, and form the knuckles of the hand. The proximal phalanges are the Radiographs of the wrist and hand are generally used to assess skeletal age. Between the elevated sternal ends of the clavicles is the jugular notch (suprasternal notch). It is grasped when testing movements of the glenohumeral joint to immobilize the scapula. The head of the humerus is surrounded by muscular tissues, except inferiorly; consequently, it can be palpated solely by pushing the fingers well up into the axillary fossa (armpit). In this position, the larger tubercle is essentially the most lateral bony level of the shoulder and, together with the deltoid, provides the shoulder its rounded contour. The lesser tubercle of the humerus could also be felt with issue by deep palpation by way of the deltoid on the anterior facet of the arm, roughly 1 cm lateral and barely inferior to the tip of the coracoid course of. The knob-like medial epicondyle, projecting posteromedially, is more prominent than the lateral epicondyle. The posterior border of the ulna, palpable throughout the length of the forearm, demarcates the posteromedial boundary between the flexor�pronator and the extensor�supinator compartments of the forearm. Because the radial styloid course of extends extra distally than the ulnar styloid process, more ulnar deviation than radial deviation of the wrist is feasible. Proximal to the radial styloid course of, the anterior, lateral, and posterior surfaces of the radius are palpable for a number of centimeters. The dorsal tubercle acts as a pulley for the long extensor tendon of the thumb, which passes medial to it. The heads of these bones kind the knuckles of the fist; the 3rd metacarpal head is most distinguished. Clavicular fractures are especially frequent in youngsters, and are often brought on by an oblique force transmitted from an outstretched hand via the bones of the forearm and arm to the shoulder during a fall. The weakest a part of the clavicle is the junction of its middle and lateral thirds. The trapezius muscle is unable to hold the lateral fragment up owing to the burden of the higher limb; thus, the shoulder drops. This fracture was so named as a outcome of the parts of the bone do Ossification of Clavicle the clavicle is the primary lengthy bone to ossify (via intramembranous ossification), beginning during the fifth and sixth embryonic weeks from medial and lateral major ossification centers that are shut collectively within the shaft of the clavicle.
Discount 500mcg fluticasone overnight delivery
The anesthetic must be injected slowly to prevent stripping of the mucosa from the hard palate. Nasopalatine Block the nasopalatine nerves may be anesthetized by injecting anesthetic into the incisive fossa in the hard palate. Paralysis of Genioglossus Greater Palatine Block the higher palatine nerve may be anesthetized by injecting anesthetic into the greater palatine foramen. The nerve emerges between the 2nd and the 3rd When the genioglossus muscle is paralyzed, the tongue tends to fall posteriorly, obstructing the airway and presenting the danger of suffocation. The tongue deviates to the paralyzed aspect throughout protrusion due to the action of the unaffected genioglossus muscle on the opposite facet. Caution should even be taken to not injure the lingual nerve when incising the duct. This particular type of radiograph (sialogram) demonstrates the salivary ducts and some secretory units. � the oral cavity (and particularly the oral vestibule) is bounded by the lips and cheeks, which are versatile dynamic musculofibrous folds containing muscles, neurovasculature, and mucosal glands, covered superficially with pores and skin and deeply with oral mucosa. � Branches of the maxillary (greater and lesser palatine arteries) and facial (ascending palatine artery) arteries supply the palate; its venous blood drains to the pterygoid plexus. � Its extrinsic muscles primarily management its placement, whereas its intrinsic muscular tissues primarily management its shape, for manipulation of meals throughout chewing, swallowing, and speech. � It is highly delicate, with 4 cranial nerves contributing sensory fibers to it. The incomplete roof of the pterygopalatine fossa is formed by the a medial continuation of the infratemporal floor of the larger wing of the sphenoid. The ground of the pterygopalatine fossa is shaped by the pyramidal process of the palatine bone. Its superior larger finish opens anterosuperiorly into the inferior orbital fissure; its inferior end narrows, persevering with as the larger and lesser palatine canals. Branches arising from the ganglion inside the fossa are thought of to be branches of the maxillary nerve. These nerves emerge from the zygomatic bone through cranial foramina of the same name and provide basic sensation to the lateral region of the cheek and temple. The pterygopalatine fossa is seen medial to the infratemporal fossa by way of the pterygomaxillary fissure, between the pterygoid course of and the maxilla. The sphenopalatine foramen is an opening into the nasal cavity at the top of the palatine bone. It conveys postsynaptic fibers from nerve cell bodies within the superior cervical sympathetic ganglion to the pterygopalatine ganglion by becoming a member of the nerve of the pterygoid canal. Communications of the pterygopalatine fossa and the passageways by which buildings enter and exit fossae are shown. The nerve of the pterygoid canal also brings postsynaptic sympathetic fibers to the ganglion from the inner carotid plexus (via the deep petrosal nerve). Secretomotor postsynaptic parasympathetic and vasoconstrictive postsynaptic sympathetic fibers are distributed to the lacrimal, nasal, palatine, and pharyngeal glands. Similarly, sensory fibers are distributed to the mucosa of the nasal cavity, palate, and uppermost pharynx. The posterior wall is then chipped away as wanted to open the anterior wall of the pterygopalatine fossa. � It is positioned between, and has communications with, the infratemporal fossa, nasal cavity, orbit, middle cranial fossa, pharyngeal vault, maxillary sinus, and oral cavity (palate). The dorsum of the nostril extends from the root of the nose to the apex (tip) of the nose. The pores and skin over the cartilages of the nostril is covered with thicker pores and skin, which accommodates many sebaceous glands. The cartilages of the nose are retracted inferiorly to expose the sesamoid cartilages. The U-shaped alar cartilages are free and movable; they dilate or constrict the nares when the muscles appearing on the nose contract.