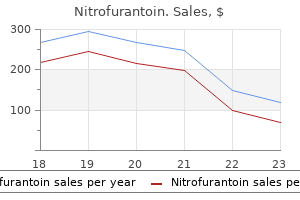
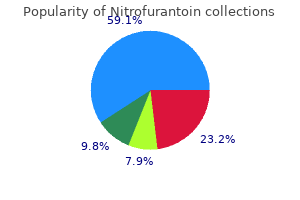
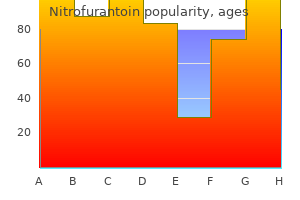
Nitrofurantoin dosages: 100 mg, 50 mg
Nitrofurantoin packs: 100 pills, 200 pills, 300 pills, 400 pills, 500 pills, 600 pills

Discount 50mg nitrofurantoin overnight delivery
Epidemiology and administration of hypertension in paediatric and young grownup kidney transplant recipients within the Netherlands. Antihypertensive pharmacotherapy and long-term outcomes in pediatric kidney transplantation. Early posttransplantation hypertension and poor long-term renal allograft survival in pediatric sufferers. Ambulatory blood strain, left ventricular hypertrophy, and allograft perform in children and young adults after kidney transplantation. Masked hypertension and allograft perform in pediatric and younger adults kidney transplant recipients. Blood pressure profiles 5 to 10 years after transplant in pediatric strong organ recipients. Dyslipidemia after pediatric renal transplantation-The impact of immunosuppressive regimens. High prevalence of the metabolic syndrome and related left ventricular hypertrophy in pediatric renal transplant recipients. He S, Le N, Frediani J, Winterberg P, Jin R, Liverman R, Hernandez A, Cleeton R, Vos M. Cardiometabolic risks range by weight standing in pediatric kidney and liver transplant recipients: a cross-sectional, single-center research in the U. Febrile urinary tract an infection after pediatric kidney transplantation: a multicenter, prospective observational study. Urinary tract infections and bladder dysfunction after renal transplantation in kids. Long-term outcomes of pediatric renal transplantation right into a dysfunctional decrease urinary tract. Vitamin D deficiency is related to brief stature and should affect blood stress control in paediatric renal transplant recipients. Mineral metabolism in European youngsters residing with a renal transplant: a European society for paediatric nephrology/european renal association-European dialysis and transplant affiliation registry examine. Franke D, Thomas L, Steffens R, Pavicic L, Gellermann J, Froede K, Querfeld U, Haffner D, Zivicnjak M. Corticosteroid use and development after pediatric solid organ transplantation: a systematic evaluation and meta-analysis. What have 20 years of data from the North American Pediatric Renal Transplant Cooperative Study taught us about progress following renal transplantation in infants, children, and adolescents with end-stage renal disease Growth impairment at renal transplantation-a determinant of growth and last peak. Metaanalysis of medical routine adherence outcomes in pediatric solid organ transplantation. Factors that influence nonadherence in immunosuppressant remedy in pediatric transplant recipients: a proposal for an educational technique. Facilitators and limitations of medication adherence in pediatric liver and kidney transplant recipients: a mixed-methods research. Tainio J, Qvist E, Vehmas R, Jahnukainen K, Holtta T, Valta H, Jahnukainen T, Jalanko H. Pubertal improvement is regular in adolescents after renal transplantation in childhood. Reliable individualized monitoring improves ldl cholesterol control in kidney transplant recipients. Omega3 fatty acids might scale back hyperlipidemia in pediatric renal transplant recipients. Infection-related hospitalizations after kidney transplantation in youngsters: incidence, risk components, and cost. Infection charges in tacrolimus versus cyclosporinetreated pediatric kidney transplant recipients on a speedy discontinuation of prednisone protocol: 1-year evaluation.
50 mg nitrofurantoin overnight delivery
Similar developments in lowered wait times and increased rate of deceaseddonor transplants with concomitant lower in livingdonor transplant in pediatric recipients have been noticed in Europe when pediatric prioritization was carried out. There was initially a noticeable decrease in transplantation price in kids <6 years of age. Due to increased threat of graft loss and mortality in infants and kids underneath 2 years of age, most pediatric facilities carry out transplants in youngsters once they achieve a weight above 10 to 15 kg. Reports from a few facilities have described successful transplant outcomes in youngsters underneath 15 kg. An further 24% of pediatric kidney transplant recipients in the identical time period obtained dialysis treatment for less than 1 year at the time of transplant. Accordingly, preemptive transplant may have quality of life advantages to youngsters beyond graft survival. Patient and Graft Survival Patient survival for pediatric kidney transplant is great, with general 5-year patient survival of ninety seven. The highest mortality for both dialysis and transplant was within the 0 to 4-year-old age group, but transplant nonetheless provided extra survival profit. However, in the past 20 years, graft survival in children of all ages now rivals the charges seen in adults. Death-censored graft survival for pediatric recipients of residing donor (A) and deceased donor (B) kidney transplants. Graft failure (D) and patient survival (E) among pediatric recipients from 2006�2010 stratified by age and donor kind. Incidence of acute rejection by 1 year for pediatric recipients over three eras, stratified by age group (in years) (C). Some of these elements are extra predictive of short-term survival, whereas others influence long-term graft survival. Donor Age and Size Multiple reports within the literature point out that donation from young adults improves graft survival. Donor age appears to be more important in figuring out graft survival for deceased-donor transplants than for living-donor transplants. Transplants from very younger donors (younger than age 5 years) to pediatric recipients have historically been averted because of stories of elevated threat of graft loss. There is a few evidence that donation from a sibling with noninherited maternal antigens confers survival benefit for the graft and could additionally be due to bidirectional immune regulation between donor and recipient immune cells. This has particular relevance for pediatrics as a outcome of mothers characterize nearly all of parental donors. It is often characterised by nephrotic-range proteinuria (protein/creatinine ratio >2 mg/mg) and hypoalbuminemia, however can present as full nephrotic syndrome, together with anasarca and hypercholesterolemia. Risk elements for graft thrombosis in kids include recipient age <6 years, donor age <6 years, chilly ischemia time >24 hours, and history of peritoneal dialysis. Situations that might not be applicable for referral or itemizing embody lively or untreated malignancy, lively or untreated an infection, and a number of or progressive medical circumstances with overall poor prognosis for recovery. Transplant is taken into account after a reasonable disease-free period for children with prior malignancies. Finally, issues with medical compliance or unstable family conditions can delay consideration for kidney transplant. Recurrence of Original Disease Recurrent illness is a significant explanation for graft loss in children, accounting for six. Biopsies early after recurrence usually demonstrate regular histology on light microscopy with effacement of podocyte foot processes on electron microscopy. It is in all probability going a multifactorial process involving cytokines secreted by T cells, a humoral issue that alters podocyte cytoskeletal structure, and a balance between circulating permeability components and inhibitors of such factors. Furthermore, demonstration of a neutralizing impact of regular serum or urine from nephrotic patients on albumin permeability suggests that loss or deficiency of a pure inhibitor could play a role. However, these studies likely overrepresent the profit of plasmapheresis given small sample sizes and using only historic teams for comparison in a few of the research or no comparability group in others. Some centers perform plasmapheresis both before a planned residing donor transplant or in the perioperative period of a deceased-donor transplant.
100mg nitrofurantoin with mastercard
An international consensus strategy to the administration of atypical hemolytic uremic syndrome in children. Outcome of renal transplantation in patients with nonShiga toxin-associated hemolytic uremic syndrome: prognostic significance of genetic background. Plasma remedy for atypical haemolytic uraemic syndrome associated with heterozygous factor H mutations. Successful isolated liver transplantation in a toddler with atypical hemolytic uremic syndrome and a mutation in complement issue H. Favorable long-term end result after liver-kidney transplant for recurrent hemolytic uremic syndrome related to an element H mutation. Successful break up liver-kidney transplant for issue H associated hemolytic uremic syndrome. Hofer J, Giner T, Cortina G, Jungraithmayr T, Masalskiene J, Dobiliene D, Mitkiene R, Pundziene B, Rudaitis S. Successful living-related renal transplantation in a patient with issue H antibody-associated atypical hemolytic uremic syndrome. Outcomes of renal transplant in patients with anti-complement issue H antibody-associated hemolytic uremic syndrome. Prophylactic eculizumab prior to kidney transplantation for atypical hemolytic uremic syndrome. Eculizumab for Atypical Hemolytic Uremic Syndrome Recurrence in Renal Transplantation. Efficacy and security of eculizumab in atypical hemolytic uremic syndrome from 2-year extensions of phase 2 studies. Outcome after transplantation of younger sufferers with systemic lupus erythematosus: a report of the North American pediatric renal transplant cooperative examine. Dialysis modality and the chance of allograft thrombosis in adult renal transplant recipients. Identifying sufferers susceptible to renal allograft thrombosis and evaluating strategies for prevention. Trends in renal transplantation rates in patients with congenital urinary tract issues. Does decrease urinary tract status affect renal transplantation outcomes in children Alexopoulos S, Lightner A, Concepcion W, Rose M, Salcedo-Concepcion K, Salvatierra O. Pediatric kidney recipients with small capability, defunctionalized urinary bladders receiving adult-sized kidney with out prior bladder augmentation. Challenges facing renal transplantation in pediatric patients with lower urinary tract dysfunction. Native nephrectomy previous to pediatric kidney transplantation: biological and clinical elements. Auber F, Jeanpierre C, Denamur E, Jaubert F, Schleiermacher G, Patte C, Cabrol S, Leverger G, Nihoul-F�k�t� C, Sarnacki S. Efficacy of nephrectomy for the remedy of nephrogenic hypertension in a pediatric inhabitants. Nephrectomy for hypertension in pediatric sufferers with a unilateral poorly functioning kidney: a contemporary cohort. Long-term cardiovascular effects of pre-transplant native kidney nephrectomy in children. Benefits of transperitoneal approach to bilateral pretransplant laparoscopic nephrectomies in pediatric sufferers. Clinical predictors of neurocognitive deficits in youngsters with continual kidney illness. Effect of conservative remedy on the renal end result of kids with main hyperoxaluria sort 1. An institutional experience of pre-emptive liver transplantation for pediatric main hyperoxaluria type 1. Complexity of pre-emptive liver transplantation in kids with main hyperoxaluria kind 1.
Order 50 mg nitrofurantoin visa
Management and outcomes after multiple corneal and strong organ transplantations from a donor infected with rabies virus. Transmission of an infection with human allografts: essential issues in donor screening. Screening for West Nile virus in organ transplantation: a medical determination evaluation. Chronic norovirus infection after kidney transplantation: molecular proof for immune-driven viral evolution. Outcomes of carbapenem-resistant Klebsiella pneumoniae an infection and the impact of antimicrobial and adjunctive therapies. Carbapenemresistant Klebsiella pneumoniae urinary tract an infection following solid organ transplantation. Outbreaks and clustering of Pneumocystis pneumonia in kidney transplant recipients: a systematic evaluation. Solid organ transplantation: hypogammaglobulinaemia and infectious complications after strong organ transplantation. What is the impression of hypogammaglobulinemia on the speed of infections and survival in strong organ transplantation Impact of genetic polymorphisms in cytomegalovirus glycoprotein B on outcomes in solid-organ transplant recipients with cytomegalovirus illness. Outcome of Clostridium difficile-associated illness in solid organ transplant recipients: a potential and multicentre cohort study. Recommendations for screening of donor and recipient prior to strong organ transplantation and to decrease transmission of donor-derived infections. Risk elements of invasive Candida and non-Candida fungal infections after liver transplantation. Mycobacterium tuberculosis infection in solidorgan transplant recipients: influence and implications for administration. International consensus tips on the administration of cytomegalovirus in strong organ transplantation. Transfusiontransmitted cytomegalovirus an infection after receipt of leukoreduced blood merchandise. Valacyclovir for the prevention of cytomegalovirus illness after renal transplantation. International Valacyclovir Cytomegalovirus Prophylaxis Transplantation Study Group. Application of viral-load kinetics to establish patients who develop cytomegalovirus disease after transplantation. Meta-analysis: the efficacy of strategies to prevent organ disease by cytomegalovirus in strong organ transplant recipients. The medical utility of whole blood versus plasma cytomegalovirus viral load assays for monitoring therapeutic response. Epstein-Barr virus and posttransplant lymphoproliferative disorder in strong organ transplantation. Effect of cytomegalovirus prophylaxis with immunoglobulin or with antiviral medicine on post-transplant non-Hodgkin lymphoma: a multicentre retrospective analysis. Solid organ transplantation from hepatitis B virus-positive donors: consensus guidelines for recipient management. Lamivudine in contrast with newer antivirals for prophylaxis of hepatitis B core antibody constructive livers: a cost-effectiveness analysis. Long-term results in human T-cell leukemia virus kind 1-positive renal transplant recipients. Donor screening for human T-cell lymphotrophic virus half: changing paradigms for altering testing capability. Multicenter comparison of laboratory performance in cytomegalovirus and Epstein-Barr virus viral load testing utilizing international standards. Updated worldwide consensus tips on the management of cytomegalovirus in solidorgan transplantation.
Discount 50 mg nitrofurantoin
Effect of indomethacin on bronchorrhea in sufferers with chronic bronchitis, diffuse panbronchiolitis, or bronchiectasis. Inhaled mannitol for non-cystic fibrosis bronchiectasis: a randomised, managed trial. Tiotropium ameliorates signs in sufferers with persistent airway mucus hypersecretion which is immune to macrolide remedy. Lung structure abnormalities, however regular lung operate in pediatric bronchiectasis. Defining pulmonary exacerbation in youngsters with non-cystic fibrosis bronchiectasis. Impact of lung illness on respiratory impedance in younger children with cystic fibrosis. The reproducibility and responsiveness of the lung clearance index in bronchiectasis. Lung clearance index is a repeatable and sensitive indicator of radiological changes in bronchiectasis. Cancer risk in 680,000 folks uncovered to computed tomography scans in childhood or adolescence: information linkage study of eleven million Australians. Respiratory bacterial tradition from two sequential bronchoalveolar lavages of the same lobe in youngsters with chronic cough. Children with chronic wet or productive cough-treatment and investigations: a scientific evaluate. Bacterial colonisation in patients with bronchiectasis: microbiological sample and threat components. A Comprehensive analysis of the impact of Pseudomonas aeruginosa colonization on prognosis in adult bronchiectasis. Adenovirus species C is related to chronic suppurative lung illnesses in kids. Respiratory viruses in exacerbations of non-cystic fibrosis bronchiectasis in youngsters. Exacerbations in non cystic fibrosis bronchiectasis: clinical features and investigations. Factors related to lung perform decline in adult patients with secure non-cystic fibrosis bronchiectasis. Postural drainage in cystic fibrosis: is there a link with gastro-oesophageal reflux Withdrawal of inhaled steroids in kids with non-cystic fibrosis bronchiectasis. Secondhand tobacco smoke publicity differentially alters nucleus tractus solitarius neurons at two different ages in creating non-human primates. Indoor air pollution from biomass combustion and acute respiratory infections in Kenya: an exposure-response study. Remediating buildings broken by dampness and mould for stopping or decreasing respiratory tract signs, infections and bronchial asthma. Members of the Massachusetts Department of Public Health: Vaccination, underlying comorbidities, and threat of invasive pneumococcal disease. Improving immunity to Haemophilus influenzae in youngsters with continual suppurative lung disease. Surgical management of bronchiectasis: evaluation and short-term leads to 238 sufferers. The radiological follow-up of aboriginal kids with bronchiectasis treated surgically or medically. Non-cystic fibrosis bronchiectasis in childhood: longitudinal growth and lung function. Longitudinal pulmonary operate of childhood bronchiectasis and comparability with cystic fibrosis.
Buy 50 mg nitrofurantoin
Outcomes of peritoneal dialysis catheter left in place after kidney transplantation. From the preliminary analysis of dying by neurologic criteria or imminent death from cardiorespiratory failure to the optimization of donor physiology before removal of organs, the intensivist plays an integral role in this first portion of the transplantation process. Although implementation of helmet laws can decrease motorcyclist mortality, the dearth of a nationwide common helmet legislation limits the effectiveness of this protective measure. Ischemia of the cerebral cortex and upper brainstem (the midbrain) results in a predominance of parasympathetic activity. Subsequently, brainstem ischemia on the degree of the pons triggers elevation of norepinephrine and epinephrine to properly above normal physiologic ranges, while leaving some practical parasympathetic nuclei. Deaths from brain injury on this population have truly doubled over the past decade 90 6 � Brain Death and Cardiac Death: Donor Criteria and Care of Deceased Donor 91 unopposed sympathetic input all through the body. These changes have very particular results throughout the body, which are best thought-about by organ system. Lavage samples from donors have demonstrated significant increases in inflammatory markers relative to nonbrain-dead controls. Pressure transmission results in an increase in left atrial strain, usually above mean pulmonary artery stress (see Pulmonary section). Intravascular volume is thus relatively low, and this decrease in preload with accompanying hypotension ends in decreased coronary perfusion. Despite these hemodynamic adjustments, gross echocardiographic modifications differ, with just under 50% of brain-injured sufferers having left ventricular systolic dysfunction, most with evidence of segmental wall motion abnormality. In addition, elevated blood return to the best atrium with systemic shunting will increase pulmonary blood circulate. Both of those adjustments end in destruction of pulmonary capillary integrity and trigger pulmonary edema and alveolar and interstitial hemorrhage. Brain death initiates an inflammatory response that Renal Kidneys also demonstrate decreased survival when obtained from brain-dead donors. This has been attributed to both inflammatory infiltrates in renal grafts and ischemia-reperfusion injury that happens as the interval of autonomic storm waxes and wanes. This ends in central diabetes insipidus, a common prevalence in braindead patients, occurring in as much as 78% of patients. The hypovolemia can worsen the already precarious hemodynamic status of the brain-dead donor, whereas the ensuing hypernatremia has a significant negative effect on renal and hepatic graft operate. Hepatic Although the liver is tolerant of extended periods of ischemia, it nevertheless is affected by both brain death-related inflammation and extended hypernatremia. The direct results of inflammation have yet to be elucidated, however biopsies after brain demise reveal increases in inflammatory cells, which may potentially enhance the chance of primary nonfunction and acute rejection. Presumably, the hyperosmolar cellular milieu established in hepatocytes whereas the donor is hypernatremic ends in osmotic harm when the liver is transplanted into a nonhypernatremic recipient. The first is direct neural tissue harm, which leads to irritation of the central nervous system. Release of inflammatory cytokines has been demonstrated locally in response to mind damage. In the half century for the explanation that Harvard Committee first reported on "irreversible coma" as a new criterion for demise, quite a few variations on the dedication of brain demise have been proposed. These had been then expounded upon by the American Academy of Neurology in 1995,20 and more recently reviewed and revalidated by Wijdicks and colleagues in 2010. Several stipulations have to be met before initiation of a mind dying examination. Complicating medical conditions which will interfere with medical assessment have to be addressed and resolved (Box 6. However, in addition to traumatic injuries, severe electrolyte disturbances (hyper- or hyponatremia, hyper- or hypoglycemia), severe acid�base disturbances (profound acidosis), and endocrine dysfunctions (profound cortisol depletion or hypothyroidism) should be recognized and corrected. This requires performing a drug display and ready for clearance 6 � Brain Death and Cardiac Death: Donor Criteria and Care of Deceased Donor 93 of any alcohol to beneath the authorized limit for driving (0. Finally, the patient must no less than have a core physique temperature >32�C before beginning the mind death examination. Severe hypothermia, outlined as core physique temperature <32�C, affects papillary light response, with full lack of brainstem reflexes at core temperatures <28�C.
Purchase generic nitrofurantoin line
On the affect of sample size on the prognostic accuracy and reproducibility of renal transplant biopsy. Outcome of kidney transplantation from high-risk donors is determined by each structure and function. Reassessment of the worth of post-vascularization biopsy carried out at renal transplantation: the consequences of arteriosclerosis. Prognostic significance of microvascular thrombosis in donor kidney allograft biopsies. Successful renal transplantation of deceased donor kidneys with 100% glomerular fibrin thrombi and acute renal failure as a result of disseminated intravascular coagulation. Donor kidney microthrombi and outcomes of kidney transplant: a singlecenter experience. Rapid resolution of donorderived glomerular fibrin thrombi after deceased donor kidney transplantation. Reversal of diabetic nephropathy in human cadaveric kidneys after transplantation into non-diabetic recipients. The destiny of glomerular mesangial IgA deposition in the donated kidney after allograft transplantation. Transplantation and 2-year follow-up of kidneys procured from a cadaver donor with a history of lupus nephritis. Transmission and determination of sort I membranoproliferative glomerulonephritis in recipients of cadaveric renal allografts. Accelerated rejection of a renal allograft associated with pretransplantation antibodies directed against donor antigens on endothelium and monocytes. Immunopathology of renal allograft rejection analyzed with monoclonal antibodies to mononuclear cell markers. Tubular expression of intercellular adhesion molecule-1 throughout renal allograft rejection. Variation in expression of endothelial adhesion molecules in pretransplant and transplanted kidneys-correlation with intragraft events. Tumor necrosis issue alpha in human kidney transplant rejection-analysis by in situ hybridization. Vascular endothelial growth factor expression and cyclosporine toxicity in renal allograft rejection. Chronic renal allograft dysfunction: the role of T cell-mediated tubular epithelial to mesenchymal cell transition. Acute and hyperacute humoral rejection in kidney allograft recipients handled with antihuman thymocyte antibodies. Prediction by postrevascularization biopsies of cadaveric kidney allografts of rejection, graft loss, and preservation nephropathy. The prognostic significance of particular arterial lesions in acute renal allograft rejection. Abundance of interstitial eosinophils in renal allografts is related to vascular rejection. Immunohistochemical analysis of the interstitial mast cells in acute rejection of human renal allografts. Acute rejection and graft survival in renal transplanted sufferers with viral illnesses. The medical and pathologic implications of plasmacytic infiltrates in percutaneous renal allograft biopsies. Infiltration of perforin-positive mononuclear cells into the rejected kidney allograft. Increased accuracy of renal allograft rejection prognosis utilizing mixed perforin, granzyme B, and Fas ligand fine-needle aspiration immunocytology. Induction of Fas-mediated apoptosis in a human renal epithelial cell line by interferon-gamma: involvement of Fas-mediated apoptosis in acute renal rejection.
Cheap nitrofurantoin 100 mg on line
This examine means that steroid withdrawal has limited effect in preventing new onset diabetes posttransplant. One-year evaluation suggested that early withdrawal of corticosteroids was protected, leading to wonderful affected person and graft survival, low acute rejection charges, and no graft loss to rejection72,seventy three Five-year results confirmed that early corticosteroid withdrawal supplies a similar long-term renal allograft survival and function; nonetheless, early corticosteroid withdrawal is associated with the next incidence of gentle, Banff 1A, steroid-sensitive episodes of rejection. Steroid withdrawal supplied improvements in cardiovascular risk elements (triglyceride, diabetes, weight gain). After a median follow-up of fifty one months (range 36�62 months), affected person survival was 97%, and graft survival was 91%. Graft perform was steady during the examine, with a mean estimated creatinine clearance of fifty seven mL/min on the finish of follow-up. This steroid avoidance regimen was associated with excellent medium-term affected person and graft outcomes and a low incidence of unwanted effects. Most 10-year outcomes had been described in a protocol incorporating discontinuation of steroids at postoperative day 7. The 10-year graft survival was 61% for dwelling donor transplant and 51% for deceased donor transplants, similar to 10-year Scientific Registry of Transplant Recipients nationwide information. The price of new-onset diabetes was highest in the high-dose tacrolimus group at 10 years (19%). Patients had been assigned on posttransplant day 8 to receive both steroid withdrawal (n = 191) or continuation (n = 195). Significantly larger tacrolimus trough ranges were observed in the steroid withdrawal group compared with the steroid continuation group at 2 weeks posttransplant, although this interaction was not seen in the African American subgroup. The median serum creatinine level at 6 months and general security profile have been similar with both regimens. Patient and graft survival and rejection rates have been nearly equivalent between whites and African Americans receiving alemtuzumab. The quality of renal function and the incidence of infectious issues had been similar between the alemtuzumab and basiliximab teams. Both corticosteroid-free regimens have been equally effective in stopping acute rejection, with the basiliximab/tacrolimus regimen offering some security advantages. There was no distinction in patient survival, graft survival, or the incidence of scientific acute rejection between the 2 groups. The mycophenolate and low-dose tacrolimus arm also had the highest graft survival price, but with reduced differences between teams over time, and the least acute rejection rate. In a similar research, low-immunologic-risk sufferers no less than four years posttransplant were randomized to tacrolimus weaning (n = 5) or continuation (n = 5). These two trials counsel that even in highly selective secure kidney recipients, tacrolimus withdrawal is to be prevented. The overall incidence of therapy failure (death, graft failure, biopsy-proven acute mobile rejection, or lost to followup) at 12 months was 18. Although a big advance in immunosuppressive therapy, this formulation had quite a few issues. Absorption was sluggish and showed a substantial quantity of intrapatient and interpatient variability, making dosing tough and rising the risk of continual rejection. This formulation improved bioavailability with extra rapid absorption and less variability in de novo and secure transplant sufferers. The efficacy of tacrolimus as an immunosuppressive agent in pediatric renal transplantation has been shown in single-center experiences and in multicenter trials. Tacrolimus was associated with improved graft perform at 1 and 2 years after transplantation. A 6-month randomized potential open parallel-group study with an open extension part was performed in 18 centers from 9 European nations to compare the efficacy and safety of tacrolimus with cyclosporine in pediatric renal transplant recipients. At 1 yr, tacrolimus remedy was related to a significantly lower incidence of acute rejection (36. At four years, affected person survival was related, but graft survival significantly favored tacrolimus over cyclosporine (86% vs. Three patients in each arm developed posttransplant lymphoproliferative dysfunction, and the incidence of diabetes mellitus was similar within the two groups. Tacrolimus was considerably simpler than cyclosporine in preventing acute rejection in pediatric renal transplant recipients.