Cyklokapron dosages: 500 mg
Cyklokapron packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

Discount cyklokapron
Poor dentition is characteristic in alcoholic or drugabusing people, and excessive dental caries may end result from decreased saliva production in sicca syndrome. Temporal muscle losing and "paper money" facial skin, owing to atrophy with telangiectasia, are signs of advanced liver disease. Xanthelasma from lipid deposits may be observed on the eyelids and skin around the orbits in sufferers with cholestatic liver disease. An extensive plexus of veins is seen emanating from the umbilical region and radiating throughout the anterior abdominal wall. Petechiae and ecchymoses replicate impaired production of clotting elements and hypersplenism in superior liver disease. Patches of white discoloration on the nails may be present in superior liver illness. Scratch marks from pruritus may be noticed on the trunk and extremities of sufferers with cholestatic liver illness. Examination of the Abdomen Abdominal distention with ascites and dilation of collateral veins owing to portal hypertension characterize florid signs of superior liver illness. Shifting dullness results from movement of ascites to the most dependent portion of the abdomen. The topic should be examined within the supine place, with percussion of the stomach from the midline toward the proper or left flank. A change from a tympanic sound to a uninteresting sound signifies a change from air to fluid, and the situation of that change identifies the floor of the fluid pool. Next, the examiner should percuss below the purpose at which dullness is elicited and ask the topic to turn towards the examiner. With the subject on his or her aspect, the examiner percusses once more at the identical level the place tympany transformed to dullness. If that spot is now tympanic, shifting dullness has been detected as a result of movement of the air-fluid boundary; this discovering supports the presence of ascites. A fluid wave may be felt by placing the medial border of 1 hand on the abdomen and tapping the right or left lateral stomach walls; the ensuing wave is felt by the primary hand. Scrotal edema and stomach wall hernias are sometimes present in sufferers with long-standing ascites. However, it could be very important notice that abdominal tenderness is frequently absent in spontaneous bacterial peritonitis. Percussion of the right upper quadrant can determine the liver span, normally 6 to 12 cm within the midclavicular line. The liver is best examined with the affected person within the supine position, arms parallel to the aspect of the body, and knees bent to relax the stomach muscle tissue. Palpation should begin in the best lower quadrant of the abdomen and transfer upward toward the rib cage in order that the liver edge is felt on the way up. In thin subjects, the liver edge could also be felt on deep inspiration, even whether it is normal in measurement. The liver can really feel exhausting and irregular, as in cirrhosis, or slightly tender, enlarged, and clean, as in acute viral hepatitis, alcoholic hepatitis, or hepatic congestion as occurs with right coronary heart failure. The liver can lengthen across the midline, and the left lobe can be felt within the epigastrium. When the placement of the edge of the liver is unclear, the scratch take a look at could also be helpful. In the presence of ascites, the liver edge could additionally be detected by exerting quick strain with the fingertips beneath the rib cage. A palpable gallbladder suggests obstruction of the biliary system, whereas tenderness elicited by palpation throughout inspiration (the Murphy sign) suggests acute cholecystitis. Marked hepatic tenderness with hepatomegaly is noticed in patients with a hepatic abscess (Chapter 142). Splenomegaly (Chapter 159) is recommended by dullness to percussion between the ninth and eleventh ribs within the left midaxillary line. A palpable spleen tip implies portal hypertension in a affected person with persistent liver illness, though an enlarged spleen additionally may be detected in acute viral hepatitis and infiltrative issues that contain both the liver and the spleen (see Table 159-5).
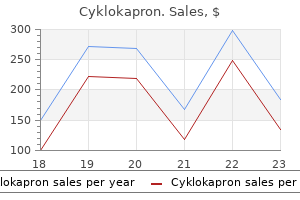
Effective 500mg cyklokapron
Correction of glossitis and different megaloblastic abnormalities within the intestinal tract may manifest as optimistic weight gain in malnourished sufferers. Recurrent macrocytosis or anemia during sufficient cobalamin substitute may counsel associated autoimmune illness, significantly thyroid issues or autoimmune hemolytic anemia. The length of and severity of symptoms earlier than treatment is inversely correlated with the extent of correction of the abnormalities. The cobalamin-deficient infant usually has residual impairments and everlasting incapacity. There is an occasional patient who develops paresthesias within the first few days after cobalamin replacement, which will resolve with further remedy. Early biomarker response and affected person preferences to oral and intramuscular vitamin B12 substitution in major care: a randomised parallel-group trial. B nutritional vitamins and hip fracture: secondary analyses and prolonged follow-up of two large randomized managed trials. Effectiveness of homocysteine reducing nutritional vitamins in prevention of thrombotic tendency at high altitude area: a randomized area trial. Vitamin B12-fortified toothpaste improves vitamin status in vegans: a 12-wk randomized placebo-controlled study. Evidence for potential underestimation of clinical folate deficiency in resource-limited countries utilizing blood tests. Absorption and blood/cellular transport of folate and cobalamin: pharmacokinetic and physiological considerations. Micronutrient deficiencies in patients with persistent atrophic autoimmune gastritis: a review. Lessons in biology from sufferers with inherited disorders of vitamin B12 and folate metabolism. Pernicious anemia related cobalamin deficiency and thrombotic microangiopathy: case report and review of the literature. Reversal of isolated 20q deletion with vitamin B12 substitute in a affected person with pernicious anaemia. Chronic proton pump inhibition therapy in the diagnostic accuracy of serum pepsinogen I and gastrin concentrations to determine pernicious anaemia. Persons of African ancestry have a really excessive incidence and prevalence of pernicious anemia. The pathology review of her peripheral blood smear documents fragmented red cells, basophilic stippling, nucleated purple blood cells, and oval macrocytes which is in maintaining with megaloblastic anemia. Flow cytometry of a bone marrow aspirate revealed increased numbers of erythroblasts and myeloblasts consistent with megaloblastic anemia. Epidemiologic investigations within the United States and Africa have documented the high incidence of pernicious anemia. Early stories from Scandinavia and Great Britain might have led to the misconceptions describing persons with pernicious anemia as largely blond and blue-eyed. As anemia worsens, megaloblastic nucleated pink blood cells and immature white cells are additionally released. Markers for early purple blood and white blood cell precursors will be increased suggesting acute leukemia as a analysis to the unwary. Transfusion could also be life-saving in such severe anemia but such sufferers as described above could have highoutput heart failure. Transfusion of washed pink blood cells may have no impression on vitamin ranges or methylmalonic acid and homocysteine levels. An 80-year-old man is now confined to a wheelchair with lack of sensation and motor weakness in bilateral decrease extremities. Recently he underwent nitrous oxide anesthesia for a cardiac procedure, and his wife noted that his signs dramatically worsened over the past 3 weeks. The severity of megaloblastic anemia and neurologic deficits as a outcome of cobalamin deficiency progress simultaneously. His history of heavy alcohol use is the most likely clarification for his elevated homocysteine value of 50 �mol/L E. His symptoms have been exacerbated by nitrous oxide anesthesia, a drug that inactivates methylcobalamin cofactor on methionine synthase within half-hour of exposure. The severity of the deficits and the length of time of deficiency previous to treatment are robust predictors of completeness of response to treatment.
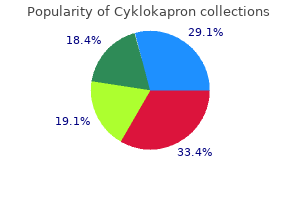
Purchase cyklokapron 500 mg online
Measurement of liver stiffness, a new noninvasive method, seems to be useful within the prognosis of cirrhosis and in excluding its presence. These tests have gotten more extensively obtainable, and typical findings on any of these imaging research, together with a compatible clinical picture, are indicative of the presence of cirrhosis. Patients with decompensated cirrhosis typically exhibit malnutrition, more extreme muscle wasting, more quite a few vascular spiders, and hypotension and tachycardia on account of the hyperdynamic circulatory state. Complications of Cirrhosis Varices and Variceal Hemorrhage Upper gastrointestinal endoscopy (Chapter 125) stays the primary method for analysis of varices and variceal hemorrhage. Varices are classified as small (straight, minimally elevated veins above the esophageal mucosal surface), medium (tortuous veins occupying lower than one third of the esophageal lumen), or massive (occupying multiple third of the esophageal lumen). The prognosis of variceal hemorrhage is made when diagnostic esophagogastroduodenoscopy shows one of the following: lively bleeding from a varix, a "white nipple" overlying a varix, clots overlying a varix, or varices with no other potential source of bleeding. Ascites Portal Pressure Measurements Direct measurements of portal pressure contain catheterization of the portal vein, are cumbersome, and may be associated with complications. Hepatic Collaterals the most typical cause of ascites is cirrhosis, which accounts for 80% of circumstances. The initial, most cost-effective, and least invasive methodology to affirm the presence of ascites is belly ultrasonography. Diagnostic paracentesis is a safe procedure that must be carried out in each affected person with new-onset ascites, even in those with coagulopathy. Depending on the medical setting, extra tests could be carried out on the fluid: glucose and lactate dehydrogenase ranges (if secondary bacterial peritonitis is suspected), smear and culture for acid-fast bacilli (if peritoneal tuberculosis is suspected), and amylase level (if pancreatic ascites is suspected). The serum-ascites albumin gradient and ascites protein levels are useful within the differential prognosis of ascites (Table 144-3). The three main causes of ascites-cirrhosis, peritoneal malignant illness or tuberculosis, and coronary heart failure-can simply be distinguished by combining the results of each the serum-ascites albumin gradient and ascites total protein content. Cirrhotic ascites sometimes has a excessive serum-ascites albumin gradient and low protein, cardiac ascites has a excessive serum-ascites albumin gradient and high protein, and ascites secondary to peritoneal malignant disease usually has a low serum-ascites albumin gradient and high protein. A excessive serum B-type natriuretic peptide has a high diagnostic accuracy in the analysis of ascites because of heart failure. Cirrhosis and its sequelae 995 Portopulmonary hypertension is diagnosed by the presence of mean pulmonary arterial stress greater than 25 mm Hg on right-sided coronary heart catheterization, provided pulmonary capillary wedge stress is lower than 15 mm Hg. Treatment of compensated cirrhosis is currently directed at preventing the development of decompensation by (1) treating the underlying liver illness. A2 Treatment of decompensated cirrhosis focuses on particular decompensating occasions and the choice of liver transplantation. Increasingly, information reveal that completely different therapies for the same complication could also be relevant to sufferers with different danger profiles, primarily primarily based on severity of the illness (see Table 144-2). Reducing portal strain decreases the risk for the event of varices and variceal hemorrhage in addition to the danger for ascites and death. In sufferers with cirrhosis and medium or giant varices that have never bled, nonselective -blockers significantly scale back the chance for first variceal hemorrhage. Ligation has no impact on portal strain and can lead to hemorrhage from ligationinduced ulcers. Screening endoscopy should be repeated each 2 to 3 years in patients with no varices, each 1 to 2 years in patients with small varices, and sooner in patients with decompensated disease in order that efficient therapy may be instituted before the varices grow in measurement and bleed. Patients with cirrhosis and variceal hemorrhage require resuscitation in an intensive care unit. Prophylactic antibiotics must be used on this setting not only to prevent bacterial infections but in addition to decrease rebleeding and demise. The really helpful antibiotic is oral norfloxacin at a dose of four hundred mg twice daily for 5 to 7 days, although intravenous ceftriaxone at a dose of 1 g/day for five to 7 days is preferable in patients with advanced liver disease (malnutrition, ascites, encephalopathy, and jaundice) or in sufferers who already are receiving norfloxacin prophylaxis. The handiest particular remedy for the control of lively variceal hemorrhage is the mixture of a vasoconstrictor with endoscopic therapy. Safe vasoconstrictors embody terlipressin, somatostatin, and the somatostatin analogues octreotide and vapreotide; they can be initiated at admission to the hospital and continued for two to 5 days. The vasoconstrictor presently obtainable in the United States is octreotide, which is used as a 50-�g intravenous bolus followed by an infusion at 50 �g/hour. The most popular endoscopic remedy to control variceal hemorrhage is esophageal variceal ligation. In instances during which bleeding continues regardless of vasoconstrictors and ligation, an esophageal stent appears to be simpler as a bridge to a more definitive therapy and is safer than balloon tamponade, although it may not cut back mortality. The differential analysis consists of conditions that worsen vasodilation, corresponding to sepsis, the utilization of vasodilators, and large-volume paracentesis not accompanied by albumin infusion; circumstances that lower efficient arterial blood volume, such as gastrointestinal hemorrhage, overdiuresis, or diarrhea (often induced by overdoses of lactulose); conditions that induce renal vasoconstriction, such as nonsteroidal anti-inflammatory drugs; and nephrotoxic insults, corresponding to from aminoglycosides.
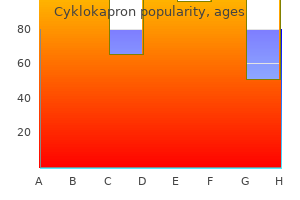
Buy cyklokapron 500 mg overnight delivery
Mesenteric angioplasty with or with out stent placement is an option in selected patients and is associated with shorter hospital stay and decrease morbidity. It is identified in about 10 to 20% of sufferers who present to the hospital with lower gastrointestinal bleeding, and its incidence is estimated at about sixteen per a hundred,000 person-years in the general population. Colon ischemia encompasses a spectrum of harm, together with reversible colopathy (most frequent, about 50%), transient colitis, persistent colitis, stricture, gangrene, and fulminant common colitis. Most cases occur in older sufferers (>60 years old), in whom the commonest trigger is transient nonocclusive hypoperfusion of a colonic section, typically without apparent cause. Although older patients are susceptible to colon ischemia in "watershed areas" of the colon (splenic flexure-descending colon), a segmental sample of involvement is frequent, most frequently involving the left colon. In younger sufferers, colon ischemia may be because of use of vasoactive substances. Most sufferers with colon ischemia present acutely with stomach pain, typically in the left lower quadrant, related to fecal urgency, diarrhea, and hematochezia. The physical examination usually reveals tenderness over the affected portion of colon, as well as belly distention. Patients with isolated right-sided colon ischemia are most likely to have more severe ache, which overshadows bleeding. As with acute mesenteric ischemia, the presence of peritoneal signs mandates immediate surgical session. About 25% of instances of colon ischemia are isolated rightside colon ischemia, which may complicate low circulate states corresponding to hypotension and sepsis, chronic kidney disease, and hemodialysis, presumably secondary to intravascular fluid shifts. No single take a look at can conclusively diagnose colon ischemia, but the analysis may be established with considered use of diagnostic modalities in the acceptable medical context. The differential analysis includes inflammatory bowel illness (ulcerative colitis and Crohn illness; Chapter 132), infectious colitis (Chapter 131), and mechanical obstruction because of colorectal most cancers (Chapter 184), fecal impaction, or stricture. Laboratory findings could also be regular, but the presence of leukocytosis and elevated blood levels of urea nitrogen and lactate dehydrogenase are indicative of a extra extreme course. Colonoscopy is the most effective check to diagnose colon ischemia, as a outcome of it permits direct visualization of the mucosal biopsy, and evaluation of the distribution and severity of the illness process. Surgery is reserved for patients with signs and signs of gangrene, perforation, or large bleeding. Patients with persistent signs have a better incidence of issues, including gangrene, perforation, segmental ulcerating colitis, and stricture. Vasculitis (Chapter 254) can involve the gastrointestinal tract, usually in association with systemic involvement. The ischemic process is typically as a outcome of immune advanced deposition that leads to the activation of complement and resulting irritation, which can then result in focal segmental ischemia. Treatment usually requires immunosuppressive drugs (Chapter 32) or surgical resection in chosen situations. Large and Medium Vessel Vasculitis Takayasu disease and big cell arteritis (Chapter 69) rarely involve the mesenteric circulation. Medium and Small Vessel Vasculitis Polyarteritis nodosa (Chapter 254) is the most typical underlying prognosis in vasculitis involving the gastrointestinal tract. The disease is characterised by segmental microaneurysms, which occur more regularly in the small bowel than in the colon. The syndrome is associated with persistent hepatitis B infection (Chapter 140) in about 50% of sufferers. Abdominal ache is the most typical symptom, however gastrointestinal bleeding and perforation have been reported. Eosinophilic granulomatosis with eosinophilia (Chapter 254) is characterised by asthma, glomerulonephritis, eosinophilia, and granulomatous irritation. Thromboangiitis obliterans (Buerger disease; Chapter 72) sometimes impacts younger males who smoke cigarettes. Mesenteric involvement is rare and often manifested by distal occlusions of the mesenteric circulation. Infantile febrile mucocutaneous lymph node syndrome (Kawasaki disease; Chapter 254) is a necrotizing vasculitis that can affect younger youngsters and trigger belly pain, ileus, obstruction, and perforation. Spontaneous perforation might happen owing to ischemia, and the illness has poor prognosis. Lupus vasculitis involving the mesenteric vessels may current with a scientific syndrome of focal segmental ischemia or continual mesenteric ischemia, however some sufferers develop vital gastrointestinal bleeding.
Generic 500 mg cyklokapron overnight delivery
The objectives of induction remedy embody a discount in the variety of acute rejection episodes in the first a number of weeks or months after transplantation, a long-term reduction in the general variety of acute rejection episodes, and a resulting improvement in long-term success charges. Despite the supply of more effective and safer immunosuppressive drugs, rejection stays an ever-present risk, and a big proportion of allograft failures are ultimately caused by immune-mediated damage. This prognosis allows for better knowledgeable decision making on the a half of both sufferers and physicians. Developing algorithms to facilitate the optimum use of suboptimal kidneys will proceed to be a challenge. These kidneys perform in addition to those recovered by conventional donation after mind death. All patients with superior chronic kidney disease have to be informed concerning the possibility of transplantation. Candidates must undergo a comprehensive medical and psychosocial evaluation to decide their suitability. The national system for the allocation of deceased donor organs in the United States is split into fifty eight donor service areas, each with an organ procurement group responsible for procuring and allocating deceased donor organs. The distribution of these organs is first native (within the donor service area), then regional, and at last nationwide if no local appropriate recipient exists. The current allocation system largely prioritizes waitlisted candidates with longest ready time as first in line for the following out there appropriate kidney within their blood group. Because of the prescreening of all donor-recipient pairs for the presence of such antidonor antibodies, hyperacute rejection happens in less than 1% of all renal transplants. Acute rejection is characterized clinically by an increase in the serum creatinine stage over days to weeks, usually within the absence of symptoms. On pathologic examination, acute rejection is most regularly "cellular" and characterized by T-lymphocyte infiltration of the tubules, interstitium, and sometimes into the vascular structures in more severe rejection. Acute rejection now happens in solely 10 to 15% of transplant sufferers through the first post-transplantation 12 months and about one other 10% within the second year. The majority of acute rejections happen within the first three to 6 months after transplantation and are clinically mild, treatable, and reversible. Percutaneous biopsy of the allograft is required to set up the prognosis with certainty, to determine the kind and severity of the rejection, and to guide therapeutic choices. Acute mobile rejection ought to be handled immediately, both with high-dose intravenous corticosteroid therapy for milder forms or with polyclonal antilymphocyte sera for steroid-resistant or extra severe acute rejection episodes. Between 10 and 20% of patients have acute antibody-mediated rejection harm, normally as evidenced by the deposition of C4d, a metabolite of a complement element C4, within the peritubular capillaries, accompanied by inflammatory cells in the peritubular capillaries. This antibody-mediated rejection may occur alone or in combination with mobile rejection. Early antibody-mediated rejection is rather more common in sufferers with a previous historical past of publicity to alloantigen via transfusion, pregnancy, or prior transplantation. The improvement of delicate reagents for detection of circulating antidonor antibodies has tremendously facilitated the diagnosis of antibody-mediated rejection. Treatment is more problematic and often entails plasmapheresis to remove antidonor antibodies and the administration of assorted regimens of intravenous 809 immune globulin. Although this treatment is usually effective in reversing acute antibody-mediated rejection, successful elimination of antidonor antibody and prevention of alloantibody resynthesis are far more tough, and chronic antibody-mediated rejection frequently follows an episode of acute antibodymediated rejection. Anti�B cell and anti�plasma cell drugs have also been tried, but none are currently approved by the Food and Drug Administration for this use. High-dose corticosteroids and polyclonal antilymphocyte serum are sometimes administered as nicely. Chronic rejection is characterised by a sluggish decline in allograft operate, usually throughout a interval of months to years, and regularly accompanied by proteinuria. Although it may possibly occur within the absence of documented episodes of acute rejection and after a few years of secure allograft function, early acute rejection is a serious risk factor for later chronic rejection and allograft failure. The improvement of donor-specific antibodies appears to be a strong threat factor for subsequent allograft failure, and antidonor antibodies are detectable in a excessive percentage of circumstances of persistent allograft dysfunction. In many sufferers with long-term deterioration of allograft function, however, the only findings are interstitial fibrosis and tubular atrophy with out clear-cut proof as to the cause.
Generic cyklokapron 500 mg on line
Steroids should be avoided as a end result of they could mask the symptoms and trigger shrinkage of the nodes in hematologic malignancies. The choice to carry out a biopsy of a lymph node is dependent upon the clinical historical past and presentation and the ease with which a biopsy can be carried out. Face-to-face discussion between the clinician and the pathologist is the most effective approach to figuring out a analysis, particularly for essentially the most difficult cases. Similar to lymph nodes, the spleen has multiple and numerous capabilities, including its function as a filter removing faulty red blood cells and infectious brokers, its necessary role in immune response to bloodborne antigens, and a task in regulating blood quantity. Consistent with its multiple features and its role as a large filter, the spleen has an open circulation with three sorts of compartments: the white pulp, marginal zone, and red pulp. Blood enters the spleen via the splenic artery and its branches, filters through the splenic cords and periarterial lymphatic sheath, and is uncovered in the white pulp to immunologically lively cells including macrophages, B lymphocytes, and T lymphocytes. There, microorganisms and international proteins are recognized, and an immune response to blood-borne antigens is initiated. In splenectomized people, the absence of this splenic operate makes them especially vulnerable to certain infections, especially these with encapsulated organisms corresponding to Streptococcus pneumoniae. More than half the volume of the spleen is composed of splenic red pulp and consists primarily of erythrocytes together with macrophages and dendritic cells and different white blood cells. Senescent or faulty purple blood cells are identified and destroyed within the pink pulp. The means of hemolysis may be mechanical and/or immunologic as in autoimmune hemolytic anemia, the place the antibody-coated pink blood cells are phagocytosed by macrophages. In the absence of a functioning spleen, basophilic inclusions representing nuclear remnants, known as Howell-Jolly our bodies, are seen in circulating purple blood cells. Last, and perhaps much less nicely appreciated, the spleen performs a task in regulating blood volume by means of quite so much of mechanisms. Whereas borderline and barely enlarged lymph nodes are commonly related to infectious causes, sizeable nodes are worrisome and warrant immediate investigation. Clearly, borderline adenopathy or lymphadenopathy associated with signs or history suggestive of a benign origin. Although most patients with lymphadenopathy come to medical consideration because they detect a lump on self-examination, an increasing number of sufferers with lymphadenopathy are identified by the way once they undergo imaging for unrelated points. An adult could determine an enlarged lymph node by way of self-examination, whereas a child might solely come to attention when there are related symptoms or the node has become easily visible to a father or mother. The location of the enlarged node(s), measurement, consistency, presence of generalized lymphadenopathy or hepatosplenomegaly, or related symptoms are all useful in creating an individualized strategy. If nodes are massive, 2 to 3 cm in dimension, and firm with associated signs, the danger for malignancy is high, and a diagnostic procedure should be performed expeditiously. A complete blood count with differential and examination of the peripheral smear together with a plain chest radiography could additionally be useful in finding out which affected person is finest served by statement for what could also be infectious mononucleosis or one other infectious and uncomplicated course of and who should proceed rapidly to biopsy. A brief course of antibiotics with close remark is usually the preferred technique with little danger if the affected person is dependable and can return if the lump grows somewhat than regresses. Splenomegaly (indicated by arrow) in a affected person with hemophagocytic lymphohistiocytosis. As with lymphadenopathy, the differential diagnosis of splenomegaly is broad ranging (Table 159-5). First, a cautious history and physical examination, with attention to the age of the affected person, the dimensions of the spleen, and related symptoms will often but not all the time guide the investigation to the underlying cause. Again, the final classes of infection, autoimmune problems, and malignancy cowl nearly all of cases. Geography and travel history are sometimes important clues to an underlying infection. The more than likely causes of splenomegaly in equatorial Africa or in a latest African immigrant are different from these of a North American urbanite. Bacterial infections commonly related to splenomegaly include endocarditis, brucellosis, typhoid fever, and rickettsial issues such as Rocky Mountain noticed fever.
Discount 500 mg cyklokapron overnight delivery
Although these two situations have totally different risk factors and natural histories, in each situations (Table 143-1) the hepatocytes are characterized by macrovesicular steatosis, which is the accumulation of triglycerides as one giant cytoplasmic globule that displaces the nucleus. In microvesicular steatosis, cytoplasmic accumulation of fats happens as a number of small globules with a central (intact) nucleus. Alcoholic liver disease is a spectrum of persistent liver illnesses starting from alcoholic fatty liver to alcoholic hepatitis and cirrhosis. Alcoholic fatty liver disease will develop in practically 90% of people who eat alcohol closely (on common, >6 drinks per day), but solely a subset of individuals develop the extreme situations of alcoholic hepatitis and alcoholic cirrhosis. Alcoholic liver disease comprises a spectrum, starting from alcoholic fatty liver to alcoholic hepatitis, alcoholic cirrhosis, and associated liver failure and most cancers. Heavy drinking is clearly the most important threat factor, whereas malnutrition and genetic factors could play a job within the illness development and decompensation. For nonalcoholic fatty liver illness, the spectrum ranges from fatty liver to steatohepatitis and associated cirrhosis, to liver failure, and to most cancers. Patients with alcoholic liver disease may have indicators and signs from underlying alcoholism as properly as those brought on by liver illness. Patients with alcoholic fatty liver illness are usually asymptomatic, however some patients might have anorexia, fatigue, proper higher quadrant discomfort, and tender hepatomegaly. Patients with alcoholic hepatitis could have a extra dramatic presentation with extreme malaise, fatigue, anorexia, fever, evidence of protein-calorie malnutrition, and features of decompensated liver illness, together with jaundice, coagulopathy, ascites, and encephalopathy. Common hematologic abnormalities embody leukocytosis with neutrophil predominance, macrocytic anemia (Chapter 155), thrombocytopenia (Chapter 163), and prolonged prothrombin time. Serum electrolyte abnormalities together with hypokalemia (Chapter 109), hypomagnesemia (Chapter 111), hypocalcemia (Chapter 232), and hypophosphatemia (Chapter 111) are frequent. Patients with alcoholic cirrhosis have the same clinical options that are common to other types of cirrhosis (Chapter 144) but additionally with hanging options of underlying continual alcoholism, together with significant muscle wasting. The prognosis of alcoholic liver disease strongly depends on the history of excessive alcohol consumption and the presence of liver illness. Serology testing for coexisting chronic viral hepatitis (Chapter 140) is crucial. Diagnostic dilemmas arise when a affected person denies extreme alcohol consumption within the face of medical features that are suggestive of alcoholic liver disease. Interviewing relations about particular alcohol consumption may be useful in the correct ascertainment of alcohol consumption. Hepatic imaging by ultrasound, computed tomography, or magnetic resonance imaging will show changes in keeping with hepatic steatosis or more superior types of liver illness, corresponding to cirrhosis and portal hypertension. Imaging can additionally be necessary to exclude different forms of liver illness, together with malignant disease and biliary obstruction. Imaging findings particular for alcoholic liver illness embrace an enlarged caudate lobe, larger visualization of the right posterior hepatic notch, and focal fats sparing or geographic fats distribution. Because particular therapy for alcoholic hepatitis may be dangerous in sufferers with different liver ailments, it is important to exclude other predominant or coexisting liver illnesses, together with chronic viral hepatitis (Chapter 140) and drug-induced liver damage, especially from acetaminophen (Chapter 141), by history, blood tests, and biopsy if needed. Hyperferritinemia typically displays an acute phase reactant, somewhat than an iron overload disorder, so it normally will return to regular when the acute liver harm resolves. Liver biopsy is the key to distinguishing alcoholic liver disease from other entities, characterizing the character of the alcoholic liver disease, and determining whether a affected person has fatty liver or extra advanced alcoholic hepatitis. In alcoholic hepatitis, the biopsy is extra hanging and reveals macrovesicular steatosis, lobular neutrophilic infiltration, Mallory hyaline, balloon degeneration of the hepatocytes, and perivenular fibrosis. In basic, patients with alcoholic hepatitis even have histologic proof of continual liver injury within the form of extra superior fibrosis (periportal or bridging fibrosis or cirrhosis). However, long-term abstinence is difficult to achieve, so a multidisciplinary method with counseling and medications that promote abstinence ought to be thought of. Alcoholic fatty liver illness requires no particular treatment aside from abstinence. Patients with alcoholic hepatitis, however, have increased short- and long-term mortality and ought to be considered for therapeutic interventions in addition to mandatory abstinence.