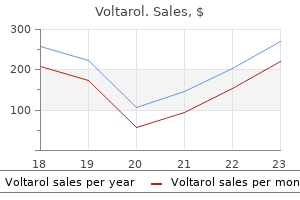
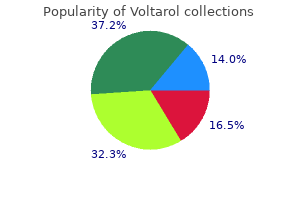
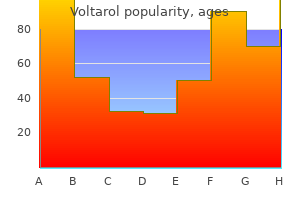
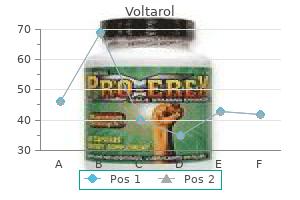
Voltarol dosages:
Voltarol packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Discount voltarol on line
Complications embody fever (transient), ulceration, stricture, perforation (rare), chest pain, mediastinitis and pleural effusion. The varix is aspirated into the banding chamber and the band placed over the varix utilizing a trip-wire mechanism, ligating the vessel. Of these sufferers, 30% will suffer gastrointestinal haemorrhage inside 1 yr of prognosis; the index variceal bleed is related to a 30�50% mortality fee. Bleeding threat is elevated in sufferers with larger varices, high portal venous pressure (>12 mmHg) and severe liver illness. Two small trials (patient numbers of 12 and 13) reported haemostasis rates of 100% and 92% and rebleeding charges of 27% and 0%, respectively. Potential risks of thrombin endotherapy embrace allergic reactions or thromboembolic issues. Gastric varices Bleeding from gastric varices solely accounts for 10�36% of all variceal haemorrhages, but the bleeding may be more extreme and the administration tougher. Therapy should be initiated as soon as variceal haemorrhage is suspected, prior to endoscopy. Produces � vasoconstriction without important systemic vascular effect or issues. Administered at an initial bolus dose of two mg every four hours, titrated all the way down to 1 mg every 6 hours after haemostasis is achieved. Contraindicated in sufferers with ischaemic coronary heart disease, terlipressin has longer organic activity and fewer unwanted effects than vasopressin. Combined vasoconstrictor and endoscopic remedy is superior to endotherapy alone; terlipressin mixed with endoscopy showed improved haemostasis and reduced mortality compared with endotherapy plus placebo. Patients ought to obtain somatostatin and its analogues at preliminary presentation with variceal bleeding; therapy ought to continue for 3�5 days following endotherapy. Management of uncontrolled variceal haemorrhage Despite urgent pharmacological and endoscopic therapy, uncontrolled haemorrhage or early rebleeding happens in 10�20% of patients. Initial emergency measures to management huge blood loss ought to be followed by definitive second-line administration of the underlying trigger. Balloon tamponade this procedure is a short lived salvage remedy for uncontrolled variceal bleeding, two balloon systems are commonly used. A meta-analysis of 12 trials evaluating antibiotic prophylaxis in cirrhotic patients with higher gastrointestinal bleeding demonstrated a vital discount in an infection rates, rebleeding and general mortality. Linton tube � with a large gastric balloon of 300�700 mL capacity which is pulled against the diaphragmatic hiatus with traction and disconnects the high-pressure portal venous system from the thoracic azygous veins. As the usage of the oesophageal balloon increases the danger of problems with little evidence of extra haemostatic effect, we should discourage its routine inflation. Haemorrhage of the severity to warrant use of a tamponade tube should also immediate consideration of elective tracheal intubation to prevent aspiration. Balloon tamponade should solely be used as a temporizing measure (12�24 hours) in sufferers with uncontrolled haemorrhage; definitive endotherapy or portosystemic shunting could be carried out as quickly as the affected person is stabilized. Secondary preventative measures ought to be commenced prior to discharge from hospital. Endoscopic remedy Repeated courses of endotherapy (at weekly intervals) results in obliteration of oesophageal varices by fibrous tissue, this normally requires two to 4 periods. Once eradicated, patients ought to bear surveillance endoscopy each 3�6 months to display for variceal recurrence. Complications happen in approximately 14% of patients however are comparatively minor, with transient dysphagia and chest discomfort occurring most frequently. A information wire is passed through the inner jugular vein into the best hepatic vein; the wire then passes by way of a needle by way of the liver parenchyma into the portal vein. A metal stent is then deployed across the intrahepatic parenchymal tract to kind a shunt between the portal and hepatic veins. Procedure-related problems embody pneumothorax, puncture site haematoma or arteriovenous fistula formation, cardiac arrhythmias, haemorrhage, arterial and bile duct damage. Postprocedure problems embrace hepatic encephalopathy, shunt-related haemolysis and stenosis or occlusion of the shunt.
Buy cheap voltarol 100 mg on-line
Thus, investigations for metastases ought to be restricted to sufferers with signs suggestive of metastatic relapse. Detection of native recurrence Relapse within the chest wall after mastectomy or in the axilla or supraclavicular fossa is normally detected clinically. Local recurrence after conservation happens at a relentless rate every year, therefore follow-up ought to be continued to 10 years. Following mastectomy the risk of local recurrence is greatest within the first 2�3 years and reduces thereafter. Although these relapses may be found at a routine hospital go to, they might even be found by the patient between visits. Relapse in the treated breast (following conservation treatment) could additionally be discovered clinically or (more commonly) on follow-up mammography. Relapse in the contralateral breast Breast cancer in one breast is related to an ~1% every year increased threat of developing most cancers within the contralateral breast. The different breast ought to due to this fact be examined at each visit and a mammogram performed each 1�2 years. Morbidity of remedy Follow-up is also a chance to assess the morbidity of therapy, especially locoregional or systemic effects. Arm mobility Women with breast most cancers could develop arm stiffness instantly associated to their surgical procedure and radiotherapy. Women undergoing breast and/or axillary surgery want shoulder exercises to enable them to recuperate a full vary of arm and shoulder mobility. Thus, all patients present process surgery and/or radiotherapy therapy to the axilla should obtain pretreatment information on lymphoedema. The incidence of lymphoedema has been cited at between 5% and 60%, relying on treatment combinations. The best management and maintenance comprises multimodal bodily therapy (skin care, external support, exercise, massage) and training. Lymphoedema ought to be handled at the first signal of swelling when management will be simpler. The lymphoedematous arm is prone to streptococcal infection after minor harm. Some studies present that progestogens corresponding to megestrol acetate and soya protein are useful in alleviating menopausal signs. Women ought to be informed relating to the potential impact of cancer treatment on their menopausal standing, and suggested relating to non-oestrogen alternatives and self-care strategies which may alleviate their signs. Prostheses External breast prostheses are the most common methodology of restoring breast symmetry following surgical procedure, and all kinds of styles and sizes can be found. A delicate momentary breast prosthesis must be fitted earlier than hospital discharge, and a permanent prosthesis should be fitted either 6�8 weeks postoperatively (or when the wound is fully healed) or following completion of radiotherapy once any pores and skin response has resolved. Menopausal symptoms Menopausal symptoms are a acknowledged issue for girls with breast cancer. Many ladies who obtain remedy for breast cancer subsequently expertise menopausal signs, both as a outcome of their adjuvant remedy or as a natural process. Breast cancer is a high-profile disease, the development and therapy of which leads to substantial bodily and psychological morbidity. Breast care nurses and voluntary sector organizations can provide verbal, written and multimedia info. Studies of the bodily impact of screening and genetic counselling appear to be reassuring. Hence, some girls choose mastectomy, although not all ladies want to share within the decision-making. Significant numbers of women develop psychological issues after anticancer therapy therapy and a few require formal treatment. Psychological components might affect the course of malignant disease however can certainly be harnessed to combat the side effects of therapy, notably chemotherapy.
Buy cheap voltarol
Isolated internal mammary chain recurrence is uncommon and supraclavicular recurrence is a manifestation of metastatic relapse. Adjuvant radiotherapy Radiotherapy has been used after surgical procedure for breast most cancers for decades. Indeed the move from radical mastectomy was facilitated by trials displaying that easy mastectomy and radiotherapy produced results equivalent to radical mastectomy, with much less lack of function. A technology later, trials confirmed that, for sufferers with small operable tumours, wide native excision and postoperative radiotherapy had been equivalent in phrases of survival and native control to conventional mastectomy. Postoperative radiotherapy is now used following mastectomy (selectively) or breast conservation for operable breast cancer. Radiotherapy after breast conservation All studies have shown that radiotherapy to the breast following limited breast surgical procedure reduces the risk of local recurrence. The absolute profit will depend upon the danger of recurrence: thus, if the danger of recurrence with out radiotherapy is 39%, this might be reduced to 13% with radiotherapy, an absolute good thing about 39% � 13% = 26%. Conversely, a danger of recurrence of 3% would be lowered to 1%, an absolute good thing about 2%. The former would definitely be clinically useful, whereas, for the latter, the toxicities of radiotherapy would most likely outweigh the (modest) profit. Adjuvant systemic remedy 399 fee with out radiotherapy is much less (albeit at the price of an impaired cosmetic result). Nevertheless, even with more in depth surgical procedure, radiotherapy significantly reduces the native recurrence price. If the affected person has systemic adjuvant remedy as well as surgery, radiotherapy additional reduces the risk of local recurrence; the magnitude of the impact is similar to that seen after mastectomy. Nevertheless, absolutely the advantage of radiotherapy for (especially older) patients with small, grade 1, node-negative breast cancers is small and there are ongoing trials quantifying this danger. Most recurrences after breast-conserving surgical procedure happen within the tumour bed and hence some research have checked out whether radiotherapy to the tumour mattress alone may be enough when it comes to native control. The good factor about the boost was primarily in patients at greater threat of recurrence (mainly youthful patients, i. Patients can anticipate a level of skin erythema and fatigue throughout and shortly after radiotherapy to the breast. In the long run, a small number of patients develop breast oedema and/or fibrosis. As talked about earlier, radiotherapy to the axilla could cause lymphoedema, particularly if given after axillary clearance. Systemic therapy for breast cancer Breast most cancers was the primary cancer to be handled systemically when Beatson reported the benefits of oophorectomy for young patients with advanced breast most cancers in 1896. Most patients will obtain some form of systemic therapy, whether this be adjuvant or palliative in intent. Effect on survival Although the significance of native remedy (surgery, radiotherapy) on native management has lengthy been acknowledged, the concept of breast most cancers as a systemic disease at presentation used to discount the importance of local therapy in phrases of survival. Longer follow-up (>15 years) has also proven a modest however real excess in overall mortality with an extra of deaths from coronary heart disease and lung cancer in irradiated sufferers. These trials have been inevitably started decades in the past (1960s and 1970s), when radiotherapy methods were very completely different, so one would anticipate (and hope) that fashionable techniques that limit the quantity of heart and lung irradiated can be safer. There is thus good proof that enhancing native control can have an result on survival, presumably by the recurrence acting as the primary focus for metastatic reseeding. The sensible implications are that native management is important and wishes meticulous technique by each surgeon and radiotherapist to decrease morbidity, maximize native control and hence enhance survival. The rationale of systemic adjuvant remedy given after surgery is to deal with and hopefully eradicate the occult distant metastases and hence improve survival. These confirm that adjuvant endocrine, cytotoxic and organic remedy can improve each recurrencefree and total survival in a subset of patients with clinically localized illness. The principles and magnitude of the benefits of adjuvant therapy could be illustrated by considering the results of trials of ovarian ablation. Finally, the usage of neoadjuvant therapy has become a powerful tool in drug improvement as it offers the opportunity to obtain tissue earlier than and after therapy to correlate tumour response with molecular parameters of drug response. Online or related packages, and molecular testing as an aid to decision-making (see web page 385). Endocrine therapy In most women, defining menopausal standing is usually simple.
Buy cheap voltarol 100mg on line
The Mallory�Weiss syndrome is widespread and accounts for 5�10% of sufferers present process endoscopy for haematemesis. The lesion consists of a longitudinal mucosal tear involving the mucosa alone or the mucosa and submucosa on the gastric facet of the oesophagogastric junction. The tear, which may be single or multiple, is located on the lesser curve side in the majority of instances (85%). Associated lesions are present in 75% of sufferers and embody hiatal hernia, oesophagitis, oesophageal varices and duodenitis/peptic ulceration. Although the bleeding stops spontaneously in the majority of patients, it may be extreme and recurrent. The situation is extra usually found in males with a historical past of alcoholism but not invariably. Endoscopic therapy is reserved for patients with actively bleeding tears at the time of endoscopy. Surgical Benign oesophageal strictures 539 Atrio-oesophageal fistula this is a rare condition that typically occurs 2 weeks following cardiac interventions. In these cases the majority of patients present with severe sepsis, cerebral abscesses and diminished stage of consciousness that requires admission to the intensive care unit. In addition to supportive measures, reported instances who survived the situation underwent surgical intervention to repair the center and oesophagus. The stricture is attributable to chronic fibrosis and scarring in response to chronic reflux damage in the decrease oesophagus. Benign oesophageal strictures occur following radiation therapy to the chest and mediastinum. Oesophageal strictures may also outcome from chemoradiotherapy treatment of squamous cell carcinoma of the oesophagus. It is crucial in these circumstances to differentiate between fibrotic benign strictures from recurrent cases and those with residual disease. Resection of at least 50% of the oesophageal mucosal circumference is strongly associated with stricture formation. Patients with strong histories of tobacco use may also be extra prone to develop oesophageal strictures following endoscopic mucosal resections. Benign strictures of the oesophagus happen following oesophageal variceal sclerotherapy in up to 30% of sufferers and fewer generally following oesophageal variceal ligation. The long limbs of the band used to occlude the oesophageal lumen are brought out via the lower finish of the incision. It consists of suture ligation of the bleeding mucosal tears via a beneficiant gastrostomy. Percutaneous embolization of the left gastric artery could additionally be utilized in poor threat sufferers similar to cirrhotic people. It may occur either spontaneously or following transoesophageal echo and cardiac ablation in patients having anticoagulation therapy. In spontaneous circumstances, it arises from an oesophageal mucosal tear related to submucosal bleeding with dissection of this airplane by the expanding intramural haematoma. Patients give a historical past of gagging or choking while eating, adopted by sharp mid-epigastric/lower retrosternal pain radiating to the back and related to haematemesis. These strictures are often long and may involve the entire size of the oesophagus. Rarely, connective tissue disorders such as scleroderma are associated with benign oesophageal strictures. Hydrophilic guide wires are likely to be much less rigid and more expensive however easier to move by way of long and tortuous strictures. When the information wire is in position the endoscope may be withdrawn and the dilators passed over the information wire across the strictured a part of the oesophagus. Advancement of the dilator must be coupled with rotation of the dilator around the information wire. For severe strictures the dilatation requires to be gradual and the process could necessitate two or extra periods with relaxation intervals of 1�2 weeks between sessions.
Order voltarol 100 mg with visa
The normal remedy is by colonoscopic decompression, which is profitable within the majority of sufferers. Surgical intervention with tube caecostomy is undertaken when colonoscopic remedy fails. They latter might end result from a motility disorder, diabetes mellitus, hypothyroidism, malignancy, psychosis or drug and laxative abuse. It is commonly assumed that hyperplasia of the lymphoid patches in the terminal ileum secondary to common illness in infancy may be involved within the initiation of idiopathic intussusception in this age group. A definite seasonal incidence is noticed in infants and kids with clear peaks in the spring and summer time. This is suggestive of viral infections being the cause of the intestinal lymphoid hyperplasia. Intussusception is anatomically defined as ileoileal, ileocaecal and ileocolic depending on the site and extent of the telescoping observed by the time of prognosis. The situation is a strangulating sort of intestinal obstruction and, if therapy is delayed, ischaemic necrosis of the involved bowel segments and peritonitis are inevitable. The scientific features include the sudden onset of vomiting, cramp-like abdominal pain and rectal bleeding. In the absence of peritonitis and intestinal obstruction, the initial treatment is by hydrostatic barium enema, which is successful in 50% and is adopted by a recurrence fee of 6%. Operative therapy is important when the hydrostatic discount is incomplete, unsure or contraindicated (peritonitis, intestinal obstruction). Operative reduction is usually potential, though the viability of the bowel may be compromised after reduction and resection is therefore needed. In adults, it has to be assumed that a lead point is present and its nature decided by subsequent investigations after restoration, until of course the lesion is palpable through the bowel wall after reduction. Volvulus Volvulus is a twist or rotation of a loop of gut about its mesenteric attachments. It is therefore a sudden obstruction of the closed loop variety if the rotation is full (360�) and ischaemia or total vascular occlusion could also be current by the time of diagnosis. Primary volvulus outcomes from malrotation of the gut or congenital extreme mobility from loose fixation or long mesenteric attachments (volvulus of the mid-gut in the neonate). The extra frequent secondary volvulus is due to rotation of a loop of small gut round an adhesions/band, an ileostomy or colostomy. The condition is encountered mostly in childhood with a peak incidence at four months. Intussusception could, nevertheless, be encountered in the adult, during which case a precipitating lesion that initiates the intussusception (the lead point) is usually present. By contrast, in infants and youngsters some 70�95% are classed as idiopathic (no lead point) and an related sickness, similar to urinary tract an infection or gastroenteritis, Intraperitoneal adhesions Adhesions following abdominal and pelvic surgical procedure are important in view of their morbidity and frequent hospital readmissions. Surgical gloves either incorporate a hydrogel polymer or are powdered with epichlorohydrinated cornstarch. There is some proof that some postoperative adhesions develop on a background of ischaemia within the area of surgically constructed anastomoses and following attempts at reperitonealization of uncooked areas. Fibrin deposition is the initiating step as that is important for mesothelial repair. Disturbance of this fine stability between mesothelial restore and fibrinolysis by ischaemia and different elements is believed to be responsible for adhesion formation after belly surgery. As the fibrinolytic exercise is compromised, the fibrin matrix persists, turns into invaded by fibroblasts and progressively matures into fibrous bands, usually within 5�7 days. Adhesions could also be parietal (between viscera and abdominal partitions and diaphragm) or visceral (between bowel loops and stable organs). They could be filmy, dense or string-like, and of variable unfold inside the peritoneal cavity, however are normally centred on the operative web site and the parietal entry wound. From the symptomatic and pathological viewpoint, parietal adhesions (those binding the intra-abdominal contents to the parieties) are more necessary than interloop/visceral adhesions. Adhesions after elective surgical procedure Although estimates of the incidence of adhesions differ (40�97%), all the reports indicate that the problem is substantial and results in both a significant morbidity and major added healthcare prices. In one retrospective cohort examine based on validated data of patients undergoing open stomach or pelvic surgery (29 760) from the Scottish National Health Service database in 1986, adopted up for 10 years, 34. Six per cent of all readmission through the study period have been instantly as a result of adhesions and the vast majority of these (97%) required an operation through the readmission. Small bowel obstruction developed in 25% of sufferers after whole colectomy with ileoanal pouch reconstruction in a single massive reported sequence of 1005 patients.
Syndromes
- Vomiting
- Metanephrine: 24 - 96 mcg/24 hours (some laboratories give the range as 140 - 785 mcg/24-hours)
- Dry the ears well after bathing or swimming.
- Fainting or feeling light-headed
- Use of certain medicines or vaccinations
- Glucose tolerance test
- Lack of energy
Purchase voltarol overnight delivery
They are classified into: �advantages: speedy onset, titratable dose common (except ketamine). The principles of the fast sequence induction are to minimize the time between the loss of laryngeal reflexes and the securing of the airway. It includes: nitrogen for �preoxygenation: 3�5 minutes, resulting in substitute ofoxygen shops oxygen within the useful residual capacity and enhance � benefits: safer aspect effect profile � disadvantages: lengthy onset time, could accumulate with renal and hepatic failure. Ketamine this drug is gaining in popularity, particularly in emergency and field anaesthesia. It acts as an N-methyl-d-aspartic acid antagonist and might cause profound analgesia, anaesthesia and amnesia. Its routine use is restricted because of its potential unwanted side effects, together with emergence delirium, dysphoria and hallucinations, tachycardia, hypertension and elevated intracranial strain. Airway During anaesthesia it may be very important keep an open airway owing to loss of normal tone causing the tongue and delicate tissues to obstruct the airway. Different types of airway embrace: airway reflexes �Oropharyngeal/nasopharyngeal: least likely to stimulateventilation. Inhalational routes use risky agents (sevoflurane, desflurane, isoflurane) together with provider gases (oxygen, air, nitrous oxide): (blood) �advantages: monitoring of end-tidal levels and so capillary wanted ranges; familiarity, convenience, minimal additional gear �disadvantages: emetogenic, greenhouse pollutant. Intraoperative care 103 a gap the trachea permitting of the �Tracheostomy:altogether. World Health Organization surgical safety checklist it is a worldwide initiative to cut back the number of surgical errors and problems. It has been endorsed by the Department of Health, National Patient Safety Agency and all of the Royal Colleges and, after an initial trial, has now been applied nationwide. Three separate checks are carried out: 1 Sign in: earlier than conduct of anaesthesia Patient might ventilate spontaneouslybut artificial ventilation is carried out during times of apnoea or if paralysis is used. The strategies of ventilation embrace: �bag and masks using anaesthetic circuits �hand air flow �mechanical air flow. Monitoring throughout anaesthesia There are requirements of primary monitoring that should be carried out in the course of the conduct of all anaesthetics. These apply to all procedures including local/regional and sedative strategies and should start earlier than the induction of anaesthesia and continue until the patient has totally recovered. The aims of ordinary monitoring during anaesthesia embody: �monitoring of important indicators to ensure sufficient tissue perfusion and oxygenation of anaesthesia �monitoring depthadverse events and errors. These embody: �Confirmation with patient of identity, website, procedure and consent. It is achieved by method of native anaesthetics and other agents to take away the feeling of ache from a specific space. This can be as a single injection, by placement of a catheter for continuous infusion or by intermittent administration of the drug. The indications include: pelvic and lower limb surgery can be carried out underneath a spinal block. Epidural anaesthesia is achieved by placement of a catheter in the extradural area. Normally its placement corresponds to the midpoint of the surgical scar, however it might be anyplace alongside the thoracic and lumbar backbone. The block is generally not as dense as a spinal, but can cover larger dermatomes and so makes it best for ache aid in upper belly surgery. Caudal anaesthesia includes insertion of a needle or cannula into the caudal house by way of the sacrococcygeal membrane and injection of roughly 20 mL of native anaesthetic. It is indicated for anaesthesia and ache reduction for perineal and inguinal surgical procedure. The frequent complications of neuroaxial blocks include: both immediate �failure: (catheter migration). It is generally accomplished on the L3�4 level (spinal twine terminates at L1�2 in adults) as a single injection but catheter strategies are additionally obtainable. All lower stomach, Peripheral nerve block techniques Peripheral nerves and plexuses may be blocked by local anaesthetic injection guided by landmarks, nerve stimulator or ultrasound imaging. In general surgery, probably the most commonly used blocks are ilioinguinal nerve blocks, transversus abdominis plane blocks, paravertebral blocks and intercostal nerve blocks. Transversus abdominis aircraft block Local anaesthetic is injected within the area between the fascia of internal indirect and transverse abdominis muscles to block the anterior rami of the decrease six (T7�L1) thoracic nerves. This offers good postoperative ache aid for quite so much of procedures involving the decrease stomach right down to the pubic area.
Generic 100mg voltarol with mastercard
Fabry illness is a uncommon, critical, inherited sex-linked recessive dysfunction of glycolipid metabolism (deficiency of -galactosidase A), which outcomes in abnormal deposits of glycophospholipids in the blood vessels and inside organs. Aside from a quantity of angiokeratoma, these sufferers often develop fever and painful arms and ft (acroparaesthesias) and corneal and lenticular modifications. They are susceptible to develop renal failure, strokes and hypertensive cardiovascular disease. Vascular malformations As indicated above, vascular malformations (hamartomas) are structural abnormalities which are decided throughout embryological development. In some instances, nonetheless, an arteriovenous fistula could develop, resulting in a high-flow malformation. Telangiectasia the telangiectasia lesion is named a spider naevus and consists of a dilated vessel with radiating branches. It is usually found on the face, arms and chest and, because of its vascular nature, it blanches on strain over the central feeding vessel. Hereditary haemorrhagic telangiectasia (Osler�Weber�Rendu disease) is characterized by multiple telangiectasia and is complicated by widespread bleeding and the late growth of arteriovenous pulmonary malformations. Individual spider naevi rarely require remedy but, if removing is required for beauty cause, thermocoagulation may be used. Port-wine stain the port-wine stain is a low-flow capillary malformation, typically called a capillary haemangioma or naevus flammeus. Port-wine stains on the trunk and limbs may be associated with lymphatic or venous abnormalities (Klippel Tr�naunay syndrome). Port-wine stains of the face could also be associated with underlying abnormalities of the meningeal and choroid plexus vasculature, resulting in focal seizures (Sturge�Weber syndrome). Port-wine stains are best treated using photocoagulation with a tuneable dye laser. This lightens the colour of the lesion and reduces the cobblestone impact in older lesions. Venous malformations Venous malformations are also referred to as cavernous haemangiomas. The adjoining bone might become distorted or hypertrophied in response to the blood flow via the lesion. Phlebothrombosis might develop inside the abnormality, giving rise to ache and induration of the lesion. Minor injury could lead to speedy enlargement of the vessels or the formation of the arteriovenous fistula. Treatment of venous malformations must be planned by delineating the extent of the irregular vessels. Treatment is dependent upon the size of the lesion and its anatomical web site, however might encompass intravascular coagulation, selective arterial embolization of feeding vessels or surgical resection. Capillary lymphatic malformations these lesions, also known as lymphangioma circumscriptum or verrucous haemangiomas, are generally found on the limbs and trunk. Treatment, when necessary, is by surgical excision and it is essential to take away any deep extensions of the lesion to stop recurrence. Angiokeratoma Angiokeratomata are abnormalities of the microvasculature presenting as dark red/purple spots as a lot as 1. There are 4 types: (1) sporadic, (2) angiokeratoma of Fordyce, (3) angiokeratoma circumscriptum and (4) Fabry syndrome (angiokeratoma corpus diffusum). The sporadic kind (angiokeratomata of Mibelli) types solitary lesions on the palms and toes in sufferers over forty years old. The angiokeratomata of Arteriovascular malformations Compared with low-flow abnormalities, high-flow vascular malformations are rare. They are inclined to happen on the top and neck and limbs and should come up from an harmless low-flow capillary vascular malformation. Clinically they present as a raised, heat lesion with a palpable thrill and a bruit on auscultation. The overlying pores and skin could turn into ischaemic and the lesion may haemorrhage spontaneously or on account of comparatively minor trauma.
Purchase 100 mg voltarol with amex
Peritonectomy is a surgical resolution advocated in specialist centres for some patients with helpful outcomes. Haemodialysis In the stable affected person, haemodialysis or haemodiafiltration makes use of a mix of diffusion and convection across a man-made extracorporeal membrane to take away waste fluid and solutes. The length of every session varies between sufferers however is normally between 3 and 5 hours. The success of haemodialysis is closely dependent upon vascular entry to allow blood flows of >350 mL/min required for efficient dialysis. This can be achieved by the use of an arteriovenous fistula or an arteriovenous graft, which are then needled at each dialysis session or via an indwelling central venous catheter. Fistulas are the preferred form of dialysis access and are fashioned by the surgical anastomosis of an artery and vein, often within the arm: radiocephalic and brachiocephalic and brachiobasilic. The native fistula requires a interval of 4�6 weeks to mature, and failure of formation to function charges range from 20% to 50%. Steal syndromes from distal tissues are often seen with both fistulas and grafts. If dialysis is required as an emergency without other forms of access available, then a non-tunnelled central venous catheter could also be placed; ideally, this should be converted to a tunnelled catheter at the first alternative. The tunnelled catheter is typically positioned in the inside jugular vein and is then tunnelled underneath the pores and skin on the ipsilateral side; a profibrotic cuff over the external catheter tube secures it in place. The traumatic impact of the catheter on the endothelium of the central veins may predispose in the long term to the development of a central venous stenosis. The relative benefits of whole organ pancreas and islet cell transplantation stays controversial. Perioperative acute kidney harm: risk components, recognition, management, and outcomes. Oxalate nephropathy complicating roux-en-y gastric bypass: an underrecognized reason for irreversible renal failure. British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients. Ideally, these sufferers are finest served by a pre-emptive live donation as allograft survival from a residing donor surpasses that seen with a wellmatched deceased donor organ. In immunologically competent people the invasion is determined by the product of the virulence and the dimensions of the inoculum of the pathogenic organisms. Classification and consequences of infections From a sensible standpoint infections in surgical patients are best categorized as: Nosocomial (hospital-acquired) infections afflict 3�5% of sufferers and are the most important contributors to extended hospital stay, increased prices and dying after surgical treatment. On average, a postoperative wound an infection will increase the prices of an operation by 300�400%. These postdischarge infections have assumed larger importance to the general assessment of surgical morbidity and prices with the significant increase in ambulatory and short-stay surgical care. A minimum of forty five days of follow-up is necessary to obtain a sound evaluation of wound infection rates. Community-acquired infections cover a variety, with some being primarily medical in the first instance. Thus, surgical community-acquired infections require emergency surgical remedy. In addition, nosocomial infections incur added costs and improve the discomfort and disability experienced by sufferers following elective operations. For patients who maintain serious damage and folks who require important care, infection is incessantly deadly. The onset of bacterial or fungal an infection contributes, as an unbiased causative issue, to the development of multiple organ techniques failure. The request form accompanying the specimen ought to give sufficient details and, particularly, indicate the pathogens suspected each time potential. Blood cultures ought to be obtained in duplicate, 20�30 mL per set obtained from different websites in adults. The skin overlying the venepuncture web site ought to be scrubbed with antiseptic (povidone iodine) for two minutes beforehand and sterile gloves worn to stop contamination. The wound surface ought to be cleaned with sterile water (not bacteriostatic saline) before obtaining the specimen, which is best obtained by scraping. Swabs of wounds or fluids are undependable, as they may not symbolize the fluid content of the wound accurately.
Purchase cheapest voltarol and voltarol
Surgical treatment is recommended in all instances because of the chance of intestinal obstruction and strangulation. After reduction of the contents in to the abdomen, the sack, which is normally present, is excised and restore is performed by approximating the two diaphragmatic edges with non-absorbable interrupted sutures. This hernia can be associated with cardiac anomalies as within the pentalogy of Cantrell. Disorders of the diaphragm Congenital diaphragmatic hernia the event of the diaphragm is normally full by the eighth to tenth week of intrauterine life. The prevalence of the condition can be up to one in 2100 births and the male to female ratio is 2:1. Approximately 80% of fetuses with congenital diaphragmatic hernias even have polyhydramnios and most circumstances can now be recognized by ultrasonography before the twenty-fifth week of gestation. Attempts to temporarily occlude the main bronchus of the hypoplastic lung have additionally had restricted success. In common phrases 30% of fetuses with congenital diaphragmatic hernias are stillborn. Fifty per cent of these born alive with a congenital diaphragmatic hernia additionally have other congenital malformations, most regularly of the nervous system. The association with trisomy 18, 20 and 21 and with Pierre Robin syndrome can also be documented. The majority of diaphragmatic hernias are left-sided (75%), some are right-sided (22%) and some are bilateral defects (3%). The commonest sort of diaphragmatic defect is a posterolateral hernia (90%), followed in frequency by eventration of the diaphragm (5%), and the least frequent defect being a retrosternal hernia (2%). Herniation via central tendon the deficiency within the central tendon may be located on the apex of the best or left cupola or involve the central part in relation to the pericardium. On the right facet, a hernia via the central tendon incorporates a mushroom-shaped portion of liver parenchyma, which grows through the opening and enlarges on the thoracic floor of the diaphragm. It can be simply differentiated from a primary tumour of the diaphragm by ultrasound scanning or three-dimensional imaging. In left-sided hernias the fundus of the stomach normally protrudes as an aircontaining cyst on the highest of the diaphragm. A central hernia is often related to a defect in the pericardium, and small gut can herniate in to the pericardial cavity. However, surgical repair of the opposite two defects is usually really helpful due to the danger of mechanical gastric or intestinal complications. Posterolateral hernia (through foramen of Bochdalek) these hernias are posteriorly located and are as a end result of persistence of the pleuroperitoneal canals, that are the final a part of the diaphragm to close. The hernia, which is normally left-sided, presents acutely with respiratory distress in the neonatal interval. Symptomatic sufferers present with digestive symptoms as a outcome of herniation of the colon, abdomen or small bowel. Congenital hiatal hernia that is usually the sliding type and is associated with gastrooesophageal reflux. Congenital quick oesophagus In the absence of congenital defects, gastro-oesophageal incompetence is often current in the neonate. The condition corrects itself spontaneously during the first few months of life, most likely by additional growth of the intra-abdominal oesophagus. True congenital shortening of the oesophagus in infancy and childhood is very rare. In this situation, the cardia and a big portion of the fundus of the stomach are located in the mediastinum without any apparent hernial sack or sliding. Most instances of congenital shortening of the oesophagus are acquired and end result from extended pathological reflux with fibrosis, ulceration and stricture formation. This hernia is extra widespread on the right and occurs by way of a triangular anterior defect lateral to the sternum between the sternal and costal attachments of the diaphragm where the superior epigastric artery, veins and lymphatics pass from the chest in to the stomach. It is normally asymptomatic within the Disorders of the diaphragm 529 the abdomen further in to the chest and, in excessive instances, the oesophageal stricture could also be located on the degree of the aortic arch.
Order voltarol us
The tumour consisting of each differentiated- and undifferentiatedtype carcinoma is classified according to the quantitative predominance. Diagnosis of ulcerative findings is principally based on histological proof of ulcerative findings. For a proximal gastric tumour invading the gastro-oesophageal junction, gastrectomy with decrease oesophagectomy is really helpful. If the tumour invading the oesophagus is lower than 2 cm, a complete stomach strategy with transhiatal resection of the lower oesophagus and lower mediastinal lymph nodes can be achieved. If the tumour extends more than 2 cm into the oesophagus, sufferers normally require left thoracolaparotomy. Extensive gastric tumour involving the junction greater than 2 cm usually requires whole gastrectomy with decrease oesophagectomy with Roux-en-Y oesophagojejunal reconstruction. Curative surgical procedure 1 Standard gastrectomy is the principal surgical process performed with healing intent. It includes resection of at least two-thirds of the stomach with D2 lymph node dissection. Omentectomy Removal of gastric omentum is usually integrated in normal gastrectomy for T3 or debulked tumours. For tumour penetrating the serosa or the posterior gastric wall, full bursectomy including the pancreatic capsule is performed with the aim of removing microscopic tumour deposits in the lesser sac. Bursectomy must be prevented in T1�T2 tumours to reduce chances of harm to the pancreas. Combined resection It is crucial to obtain R0 resection and therefore, for tumour invading adjacent organs, mixed resection could also be essential. Non-curative surgical procedure Palliative surgical procedure is indicated for bleeding or obstruction in sufferers with advanced gastric most cancers with unresectable metastases. Palliative gastrectomy or gastrojejunostomy is chosen depending on tumour traits and surgical threat. However, palliative surgical procedure is an extremely uncommon procedure in Western centres because of the advances of pyloric stents and oncological management. Laparoscopic surgery the advantages of laparoscopic surgical procedure in benign illness and colorectal cancer surgery have inspired surgeons to undertake this in gastric most cancers. There is a large variation in the indications of laparoscopy between the Western international locations and Japan. Small randomized control trials confirmed the potential benefit by way of general postoperative outcomes, though trials have proven no difference in major postoperative problems. It is essential to acknowledge that the aim of surgery for gastric most cancers is long-term cure. If the surgeon feels that the laparoscopic method could compromise the oncological high quality of the resection, surgeons ought to revert to the standard open approach. Extent of gastric resection A sufficient gastric resection margin must be ensured when determining the resection line in operations with curative intent. When tumours invade the gastro-oesophageal junction a 5 cm margin will not be achieved, and subsequently frozen section is really helpful to ensure R0 resection. The standard surgical procedure for clinically node constructive or T2 to T4a tumours is both whole or distal gastrectomy. Distal gastrectomy is selected when a passable proximal margin could be obtained. Pancreatic invasion by tumour requiring pancreaticosplenectomy necessitates total gastrectomy relating to the tumour location. Total gastrectomy with splenectomy ought to be considered for tumours which are situated alongside the greater curvature and harbour metastasis to 4sb lymph nodes even when the primary tumour could presumably be eliminated by distal gastrectomy. For T1N0 tumours, gastric resection could be modified as pyloric preserving gastrectomy for tumours within the middle portion of the stomach with distal tumour a minimum of four cm proximal to the pylorus and proximal gastrectomy for proximal tumours greater than half of the distal abdomen being preserved. Lymph node dissection the extent of systemic lymphadenectomy is defined based on the type of gastrectomy indicated.