Zestoretic dosages: 17.5 mg
Zestoretic packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Zestoretic 17.5mg free shipping
A case of carcinoma arising in the intrapancreatic terminal choledochus 12 years after primary excision of a large choledochal cyst. Risk of bile duct carcinogenesis after excision of extrahepatic bile ducts in pancreaticobiliary maljunction. Intrahepatic cholangiocarcinoma arising 10 years after the excision of congenital extrahepatic biliary dilatation. The choledochocele: correlation of radiological, clinical and pathological findings. Symptoms of bacterial cholangitis are much less frequent, except if the affected person has dominant biliary strictures and/or biliary stones. The bodily examination of symptomatic patients might reveal jaundice, hepatomegaly, splenomegaly, pores and skin excoriations, ascites, and peripheral edema. The most frequent clinical presentation currently is an asymptomatic affected person with persistently increased ranges of alkaline phosphatase famous on routine serum biochemical testing. Asymptomatic people usually come to medical attention because of abnormal liver biochemistry detected throughout routine screening. Symptomatic patients current with symptoms/signs of cholestasis and issues of chronic cholestatic liver disease. The signs might embody fatigue, pruritus, right higher quadrant pain, weight reduction, and manifestations associated to portal hypertension. Endoscopic dilatation and stenting is the optimal preliminary treatment of symptomatic dominant biliary strictures. Enlarged lymph nodes are often present within the porta hepatis and alongside the right and customary hepatic arteries and the hepatic and common bile duct. Unfortunately, histologic modifications may be markedly varied from section to section of the liver at any given point in time. Strictures are sometimes diffusely distributed with intervening segments of dilated ducts. The cholangiographic findings usually involve each the intrahepatic and extrahepatic bile ducts. Abdominal ultrasonography is efficacious to consider the bile ducts for dilation and/or stones, and liver parenchyma for cirrhosis. In addition, they discovered presence of dysplasia in each adenomatous and malignant lesions, supporting the adenoma-carcinoma sequence. Most importantly, their examine found no statistical distinction between the size of benign and malignant lesions. Liver biopsy exhibits moderate to severe interface hepatitis with or without biliary destruction. In the trendy era, nontransplant surgical intervention for dominant strictures has largely been replaced with endoscopic administration. Fifty sufferers underwent resection of the extrahepatic biliary tract; 40 of these sufferers have been noncirrhotic. All sufferers had symptomatic biliary obstruction, and the primary indications for treatment had been persistent jaundice and cholangitis. Postoperative issues developed in 32% of patients, the most typical being cholangitis. When endoscopy fails, surgical interventions, similar to extrahepatic biliary resection with transhepatic stenting, can be thought-about for noncirrhotic sufferers in facilities with acceptable expertise. Two well-liked options are Roux-en-Y choledochojejunostomy and choledochocholedochostomy (a duct-to-duct anastomosis). Initial publications reported that Roux-en-Y reconstruction may reduce the incidence of postoperative stricture formation and improve affected person and graft survival when compared with duct-to-duct anastomosis. Initial publications following this protocol demonstrated 5-year survival rates of 82%. Complications associated with surgical management of ulcerative colitis are highly affected by the degree of liver illness current on the time of surgical procedure. Repeated brushings can improve the sensitivity43 and are highly beneficial when the obtained materials proves suspect or adverse within the presence of high medical suspicion. The traditional classification contains double tumor, combined kind, and blended type.
Zoete Amandel (Sweet Almond). Zestoretic.
- Relieving chapped and irritated skin.
- Use as a laxative.
- Dosing considerations for Sweet Almond.
- What is Sweet Almond?
- Constipation; irritated skin; and treating cancer of the bladder, breast, mouth, spleen, and uterus.
- Are there safety concerns?
- How does Sweet Almond work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96105
Buy zestoretic 17.5mg line
Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus eight. Metaanalysis of randomized controlled trials of endoscopic retrograde cholangiography and endoscopic sphincterotomy for the remedy of acute biliary pancreatitis. Endoscopic management of cholangitis: critical evaluate of an alternate technique and report of a big collection. Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Unilateral versus bilateral endoscopic hepatic duct drainage in sufferers with malignant hilar biliary obstruction: results of a potential, randomized, and controlled research. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Metal or plastic stents for preoperative biliary drainage in resectable pancreatic cancer. A multivariable mannequin utilizing superior cytologic methods for the analysis of indeterminate pancreatobiliary strictures. Choledochocele, an ignored diagnosis: report of 15 circumstances and review of fifty six revealed reviews from 1984 to 1992. Dilated common channel syndrome: endoscopic prognosis, therapy, and relationship to choledochocele formation. Endoscopic sphincterotomy in younger patients with choledochal dilatation and a long frequent channel: a preliminary report. Endoscopic remedy in sufferers with pancreas divisum and acute pancreatitis: a potential, randomized, managed clinical trial. Long-term results after endoscopic pancreatic stent placement without pancreatic papillotomy in acute recurrent pancreatitis because of pancreas divisum. Long-term results of endoscopic management of pancreas divisum with recurrent acute pancreatitis. Interventional endoscopy within the analysis and staging of higher gastrointestinal malignancy. Endoscopic ultrasound for staging esophageal most cancers, with or without dilation, is clinically important and protected. Effect of covered metallic stents in contrast with plastic stents on benign biliary stricture decision: a randomized medical trial. Successful administration of benign biliary strictures with fully lined self-expanding metallic stents. Long-term follow-up after biliary stent placement for postoperative bile duct stenosis. Longterm outcomes of endoscopic administration of postoperative bile duct strictures with increasing numbers of stents. Endoscopic therapy of biliary tract strictures in sclerosing cholangitis: a larger collection and recommendations for remedy. Endoscopic stent therapy for dominant extrahepatic bile duct strictures in primary sclerosing cholangitis. Postsurgical bile leaks: endoscopic obliteration of the transpapillary pressure gradient is sufficient. Impact of endoscopic intervention in a hundred sufferers with suspected postcholecystectomy bile leak. Endoscopic remedy for bile leak primarily based on a new classification: results in 207 sufferers. Palliative bile duct drainage-a new endoscopic methodology of introducing a transpapillary drain. Randomised trial of self-expanding steel stents versus polyethylene stents for distal malignant biliary obstruction. A potential, randomized, managed trial of metal stents for malignant obstruction of the frequent bile duct. Plastic endoprostheses versus steel stents in the palliative therapy of malignant hilar biliary obstruction. Conventional versus Rosemont endoscopic ultrasound standards for continual pancreatitis: evaluating interobserver reliability and intertest agreement.
Discount zestoretic express
Chemotherapy with 5-fluorouracil and a platinum compound improves outcomes in metastatic small bowel adenocarcinoma. Combination chemotherapy with cisplatin and irinotecan in patients with adenocarcinoma of the small intestine. Systemic chemotherapy for remedy of superior small bowel adenocarcinoma with prognostic factor evaluation: retrospective study. Multicenter retrospective research of 132 patients with unresectable small bowel adenocarcinoma handled with chemotherapy. Immunophenotype and molecular characterisation of adenocarcinoma of the small intestine. Beclin 1 activation enhances chemosensitivity and predicts a positive end result for primary duodenal adenocarcinoma. Duodenal most cancers arising from the remaining duodenum after pylorus-preserving pancreatoduodenectomy for ampullary cancer in familial adenomatous polyposis. Chemotherapy in small bowel adenocarcinoma: 10-year experience of the British Columbia Cancer Agency. Efficacy of adjuvant chemotherapy for small bowel adenocarcinoma: a propensity score-matched analysis. Double balloon enteroscopy detects small bowel mass lesions missed by capsule endoscopy. Any operation done for these causes, whether or not laparoscopic or open, can lead to long-term complications requiring reoperation. Reoperations for obesity-related procedures shall be covered within the chapters coping with bariatric surgery. This may be made simpler if the initial procedure was accomplished laparoscopically or if a bioresorbable barrier was placed beneath the incision in open surgery. The relative infrequency of reoperative surgery and the high value of those obstacles have restricted their use. If the dissection is started just under the xiphoid course of in the midline, reentry of the peritoneal cavity is less more doubtless to trigger damage to underlying small bowel or colon. The liver and stomach underlie this area and are both much less susceptible to harm and simpler to repair than small bowel or colon. Lysis of all intraabdominal adhesions is unnecessary and may improve the probability of iatrogenic small bowel or colonic damage. The dissection ought to be restricted to the exposure needed to full the planned procedure. Early reoperation will lead to essentially the most problem because of the presence of adhesions, that are most intense within the first few weeks after the initial process. Over time, many of these adhesions resorb, and thus ready at least 6 months between the index operation and the reoperation, if potential, is advisable. The dictated operative report must be obtained and reviewed to permit an excellent understanding of the altered anatomy to be encountered. This may be additional enhanced by reviewing beforehand done imaging or endoscopic studies or obtaining extra studies if essential. An correct understanding of the anatomy to be encountered, together with the placement of intestinal limbs, will greatly assist in designing an environment friendly and successful reoperation. Many complications of operations on the stomach and duodenum that require reoperation end in important malnutrition. It is essential that this be corrected prior to the repeat operation if in any respect potential. This can be accomplished with total parenteral diet in nearly all circumstances; nonetheless, if entry to the small bowel could be obtained, enteral vitamin has some benefits. In any case, measuring prealbumin ranges and different nutritional assessment parameters, and delaying operation until they return to regular or close to normal values, can result in lower morbidity, quicker restoration, and overall better outcomes. In the setting of recurrent ulcer disease or persistence of signs after an initial operation, you will want to rule out related causes as the underlying etiology.
Purchase 17.5 mg zestoretic with visa
This is obvious even though these procedures have been performed for the most half in the absence of acute cholecystitis (91%), thus with much less irritation and theoretically better situations for proper identification of anatomic constructions. This approach has resulted in longer operative times with out important enhancements in other intraoperative or postoperative outcomes compared with normal laparoscopy. Comparing near-infrared imaging with indocyanine green to conventional imaging throughout laparoscopic cholecystectomy: a prospective crossover study. Specialist early and immediate restore of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term consequence. Major bile duct damage requiring operative reconstruction after laparoscopic cholecystectomy: a follow-on examine. Subtotal cholecystectomy for "troublesome gallbladders": systematic evaluation and meta-analysis. Timing of percutaneous cholecystostomy impacts conversion rate of delayed laparoscopic cholecystectomy for severe acute cholecystitis. A nationwide examination of outcomes of percutaneous cholecystostomy in contrast with cholecystectomy for acute cholecystitis, 1998-2010. Outcome of conservative percutaneous cholecystostomy in high-risk sufferers with acute cholecystitis and risk components resulting in surgery. Changing developments and outcomes in using percutaneous cholecystostomy tubes for acute cholecystitis. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a evaluation and a word of warning. Randomized managed trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. A randomized managed trial comparing post-operative ache in single-incision laparoscopic cholecystectomy versus typical laparoscopic cholecystectomy. Postoperative pain after transvaginal cholecystectomy: single-center, double-blind, randomized managed trial. Robotic versus laparoscopic cholecystectomy inpatient evaluation: does the end justify the means Soper holedocholithiasis is a standard condition that always requires a procedural intervention so as to treat. As such, the talk about the optimum management of sufferers with choledocholithiasis has endured for many years. In addition, the level of assist current in the health care facility to which the affected person presents usually dictates remedy options, provided that using nonsurgical options requires the presence of endoscopic and/or interventional radiology capability. Patients presenting with cholecystitis, biliary colic, pancreatitis, and jaundice have been discovered to have widespread duct stones 7%, 16%, 20%, and 45% of the time, respectively. A number of different therapy methods are employed when managing sufferers who present with choledocholithiasis. As such, the debate over the optimal management of these sufferers has persisted for a couple of years. The choice of which option to pursue depends on patient-level considerations, including the presence of comorbidities that make the risk of surgical intervention prohibitive, in addition to the timing of prognosis of choledocholithiasis. Furthermore, the extent of help present in the well being care facility to which the patient presents usually dictates remedy options, on circumstance that using nonsurgical options requires the presence of endoscopic and/or interventional radiology capability. Endoscopic papillary dilation has been suggested instead; a multicenter randomized research demonstrated that endoscopic balloon dilation resulted in the next price of pancreatitis compared with sphincterotomy and recommended that it must be averted in routine follow. Before either process, a clip is utilized high on the cystic duct at its junction with the gallbladder to stop stones migrating down the duct. A cholangiography catheter is inserted into the cystic duct and secured in place with a clip, greedy jaws, or balloon fixation. After threading the beforehand positioned guidewire via the working channel, the choledochoscope is inserted by way of a protective introducer positioned within the midaxillary port. In the transcystic duct method, small stones (<2 to 3 mm) can often be flushed by way of the ampulla into the duodenum. Intravenous glucagon (1 to 2 mg) may be used to chill out the sphincter of Oddi, adopted by vigorous flushing of a hundred to 200 mL of saline. If attempts at transcystic basket extraction fail, a choledochoscope (10 French) must be tried next to remove the stones beneath direct imaginative and prescient.
Purchase zestoretic visa
The common denominator in the pathogenesis of this syndrome is hepatic venous outflow obstruction characterised by the traditional medical triad of stomach pain, hepatomegaly, and ascites. In most circumstances the cause is an identifiable, inherited or acquired, hypercoagulable state. Hepatic vein occlusion leads to increased sinusoidal pressure and decreased sinusoidal blood flow. Diminished sinusoidal blood move is believed to be essential in the pathogenic progression of fibrosis and regenerative nodule formation leading to cirrhosis. Portal hypertension contributes to ascites formation and the development of varices. Rupture is rare however has been reported, and even spontaneous decision has been documented. The medical presentation of sufferers with Budd-Chiari syndrome varies relying on the extent and acuity of the obstruction to the hepatic venous outflow. Suddenonset, full hepatic vein thrombosis may every so often current as fulminant liver failure. The diploma to which these collaterals decompress the portal venous system impacts the clinical manifestations of the syndrome and determines the preferred remedy. Some sufferers develop liver enlargement and intractable ascites with relatively preserved hepatic function, whereas others develop cirrhosis with hepatic decompensation. Laboratory investigation of liver function might reveal abnormalities, but these checks are nonspecific. Ascitic fluid evaluation may reveal a excessive serum/ascites albumin gradient and an elevated protein stage (>3 g/dL). When the underlying cause is tumor invasion of the hepatic veins, these imaging research are necessary for figuring out the native extent of the disease. After the analysis is established, a liver biopsy may be wanted to determine the extent of hepatic fibrosis and cirrhosis. Because the hepatic parenchyma is most likely not uniformly affected, bilobar biopsies could additionally be useful to keep away from sampling error. A variety of medical therapies, interventional radiologic methods, and surgical procedures can be found for the affected person with Budd-Chiari syndrome. Medical therapies embody anticoagulation, thrombolysis, and pharmacologic treatment of ascites and portal hypertension. Surgical procedures embrace a variety of portosystemic shunts and liver transplantation. Percutaneous thrombolysis/thrombectomy alone has been attempted for acute hepatic vein thrombosis anecdotally however with restricted success. Vein angioplasty with or with out stent placement additionally has been tried in chosen instances. It is indicated within the patient with Budd-Chiari syndrome and chronic, well-compensated liver illness to relieve portal hypertension and deal with intractable ascites. For sufferers with fulminant liver failure or decompensated cirrhosis, the process has a high incidence of problems. Clinical and pathological analysis of hepatic artery aneurysm in a affected person with systemic lupus erythematosus. Hepatic artery mycotic aneurysm related to staphylococcal endocarditis with successful treatment: case report with evaluate of the literature. Fatal upper gastrointestinal bleeding because of hepatic artery pseudoaneurysm diagnosed by endoscopy. Life-threatening postoperative hemorrhage from hepatic artery pseudoaneurysm successfully treated by transcatheter embolization in a 5-year old baby. Preservation of the arterial vascularization of the hepatic artery pseudoaneurysm following orthotopic liver transplantation: long-term results. Hemobilia related to an enormous thrombosed aneurysm of the hepatic artery requiring hepatectomy. Management and consequence of sufferers with combined bile duct and hepatic arterial injuries after laparoscopic cholecystectomy. Impact of concomitant arterial harm on the outcome of laparoscopic bile duct damage. Hepatic resection for post-cholecystectomy bile duct injuries: a literature evaluation. Long-term deleterious effect of aortohepatic conduits in main liver transplantation: proceed with warning.
Buy cheap zestoretic 17.5 mg
Distal obstruction, whether mechanical or not, leads to growing bowel diameter, with rising wall rigidity resulting in native ischemia. Hypoalbuminemia represents a marker of a much wider physiologic derangement than simply malnutrition. Animal experiments have demonstrated that the body prioritizes visceral wound therapeutic over most different sources of protein consumption, together with parietal wound healing. Multiple approaches have been proven to be efficient, including surgical stapling as equally safe to suturing under many conditions. A number of older studies looked at variations between handsewn and stapled bowel anastomoses. In basic, no differences were famous within the leak fee, morbidity, mortality, and cancer recurrence. The ideal suture material for intestinal anastomosis is one that produces the smallest quantity of tissue response while providing maximal strength in the course of the lag or inflammatory part of wound healing. All sutures lead to some extent of tissue inflammation because the act of pulling the suture thread via the bowel wall causes some tissue damage. This inflammatory reaction affects ranges of activated collagenases and matrix metalloproteinases leading to decreased tensile power of the healing wound. It is crucial to avoid this energy imbalance through the crucial lag period (days 1 to 5) as the wound transitions from the inflammatory section to the proliferative section. As a monofilament suture, coupled with an acceptable needle, it allows for the least quantity of tissue injury from the act of suturing. It is slowly absorbed with good retention of energy for as much as 6 weeks, properly past the crucial lag period. The adherence of micro organism to the suture material has been postulated as a possible clarification for bacterial an infection and weakening of the intestinal anastomosis. Polydioxanone has been proven to have the bottom affinity to adherence of bacteria among the absorbable sutures. Others confirmed the diploma of infection in mice within the presence of suture correlated with the adherence properties of that suture for micro organism. Coating suture with an antibacterial agent (triclosan) significantly reduces adherent bacteria to polyglactin, is associated with decreased microbial viability and significantly increased bursting stress in colonic anastomoses. The continuous suture has the benefit of being more watertight with the drawback that the integrity of the whole suture line is predicated on one stitch. Although hemostasis can be improved with a steady suture, the converse impact, that continuous suture may constrict anastomotic blood move leading to ischemia and anastomotic dehiscence, is also true. Most human research indicate that a continuous anastomosis can be performed safely and quickly, with no important distinction between steady and interrupted suture sample. Single-layer anastomosis consists of 1 layer of interrupted or continuous absorbable sutures, whereas a double-layer typically consists of an internal full-thickness layer of absorbable suture and an outer layer of interrupted absorbable or nonabsorbable sutures. Anastomoses with the inverted technique heal faster31 with superior bursting stress and extra prompt return to regular bowel structure. It is used as the outer layer of a two-layer bowel anastomosis and can be used to restore seromuscular tears in the bowel wall. The stitch is started roughly three to four mm lateral to the incision and positioned at a proper angle to the lengthy axis of the incision ("follow the curve of the needle"). It incorporates only the seromuscular layer; care must be taken to not incorporate the complete thickness of the bowel wall. The tip of the needle is brought out close to the sting of the incision and is then reinserted in the apposing wound edge and introduced out three to 4 mm lateral to the wound edge. The suture is then tied all the method down to a tension that approximates the tissue but not tight enough to tear the tissue. The suture is passed by way of the seromuscular layer 2 to three mm lateral to the wound edge and introduced out on the wound edge; the needle is then passed by way of the opposing edge of the wound and introduced out 2 to 3 mm lateral. On that very same aspect of the wound, roughly 2 mm distal, the suture is passed via both edges of the wound to create two free ends of the suture on one side of the wound edge with the loop of the suture on the opposite side. This sew is especially useful in broken, infected, or irregular tissue where a Lembert suture pulls by way of the tissue. Because the horizontal mattress sew distributes pressure in a aircraft perpendicular to that of a Lembert suture, it allows for apposition of tissues with less crushing impact.
Syndromes
- Fever
- Have you been drinking alcohol heavily?
- Lungs
- Get drugs that suppress the immune system, such as corticosteroids or rituximab
- Travel to areas with low pollen counts
- Uses plurals and pronouns (he/she)
- Name of the product (ingredients and strengths, if known)
Purchase 17.5 mg zestoretic with mastercard
Wrapping omentum round an intestinal anastomosis to reinforce the anastomosis and foster the pure means of therapeutic theoretically allows the omentum to mechanically seal the anastomosis in adhesions and play a task in angiogenesis. Tissue adhesives are fibrin glues which would possibly be generally used for hemostasis, bone sealing, and other simple tissue repairs. They depend on the conversion of fibrinogen to cross-linked fibrin to assist in hemostasis and the reinforcement of tissue energy. In conclusion, the routine medical use of tissue adhesives for the reinforcement of bowel anastomoses has to be made with consideration. Adhesion obstacles are hyaluronic acid�based absorbable movies whose aim is to cut back adhesion formation through the regular therapeutic process. They mechanically separate adhesiogenic tissue by turning into a hydrated gel after which absorbing over the course of approximately every week. Use of a hyaluronic acid�based movie has been shown to enhance the speed of fistula formation and peritonitis in patients undergoing intestinal anastomosis. Furthermore, in a subgroup of sufferers who had the film wrapped round a recent anastomosis, anastomotic leak, fistula, peritonitis, abscess, and sepsis occurred significantly extra regularly. In 1985 a biofragmentable anastomotic ring was developed with the intention to facilitate sutureless intestinal anastomosis. The system consists of two equivalent circular rings composed of Dexon and 12% barium sulfate. Prolene sutures are used to create purse-string stitches at the two cut ends of the bowel, and the sutures are tightened across the rings after the rings are placed inside the bowel lumens. Further examine has proven this system to be secure to be used also in emergency anastomosis. Both of those devices doubtless want long-term follow-up before they will be thought-about in clinical practice for substitute of traditional anastomotic methods. Animal research utilizing a bovine pericardium patch to reinforce intestinal anastomosis have shown promising results. Use of a porcine mannequin signifies the patch is safe and efficient and demonstrated improvement in mitochondrial operate and normalization of mucosal transport after wrapping the anastomosis with the patch. Although these results are promising, future analysis must give attention to human outcomes before both patch can enter routine scientific follow. Early outcomes indicate no vital distinction when it comes to end result, leak rate, or infection for sufferers with intestinal anastomosis. Enhanced intestinal anastomotic healing with gelatin hydrogel incorporating fundamental fibroblast development factor. Laparoscopic gastrointestinal anastomoses utilizing knotless barbed sutures are secure and reproducible: a single-center expertise with 201 sufferers. The hand-sewn anastomosis with an absorbable bidirectional monofilament barbed suture Stratafix during laparoscopic one anastomosis loop gastric bypass. Bacterial adherence to surgical sutures: can antibacterial-coated sutures cut back the chance of microbial contamination The effect of various suture materials on the safety of colon anastomosis in an experimental peritonitis mannequin. Single-layer steady colon and rectal anastomosis utilizing monofilament absorbable suture (Maxon). Single- versus two-layer intestinal anastomosis: a meta-analysis of randomized managed trials. Single layer versus double layer suture anastomosis of the gastrointestinal tract. A managed trial of inverting versus everting intestinal suture in clinical large-bowel surgery. The use of staplers in anatomical side-to-side and practical end-to-end enteroanastomoses. The ideal time to resume oral feeding after intestinal anastomosis has been the topic of much debate. The preponderance of proof points to the dearth of harm, and sometimes the benefit, of early oral feeding.
Purchase 17.5 mg zestoretic mastercard
Diagnosis of liver abscess is confirmed by a constructive serologic take a look at as a outcome of amebic serology is highly delicate (>94%) and highly specific (>95%). Photograph of a gross liver specimen reveals an amebic abscess crammed with a chocolatecolored, pasty material (anchovy paste). In nonendemic areas, a optimistic amebic serology nearly all the time displays acute infection and, within the setting of hepatic abscess, is basically diagnostic of an amebic etiology. They offer the very best sensitivity and specificity and can also differentiate between the various Entamoeba species. All three methods may facilitate guided needle biopsy and drainage if indicated. The common time to radiologic decision is three to 9 months and may take years in some patients. Studies have proven that more than 90% of the seen lesions reveal disappearance on imaging, however a small share of patients are left with a clinically irrelevant residual lesion. Cerebral amebiasis has an abrupt onset and speedy development to dying in 12 to 72 hours. Amebomas are localized masses of contaminated granulation tissue in the intestine whose appearance can mimic colon cancers, and these lots can lengthen to contain the perianal skin. It is given in doses of 750 mg 3 times a day by mouth or intravenously for 5 to 10 days. The main unwanted facet effects embrace metallic aftertaste, nausea, vomiting, and diarrhea. The medicine for amebic colitis embody luminal agents, such as paromomycin, which is the drug of alternative; diloxanide furoate; and iodoquinol. The standard indications for percutaneous drainage embrace deterioration in scientific condition on sufficient remedy, bacterial superinfection, and an abscess having a excessive threat of rupture, whereas surgery is reserved for patients with ruptured abscess, impending rupture, or insufficient drainage by way of a catheter. Hospital stay in the aspiration group was longer than that in the nonaspiration group, and no statistically vital distinction in mortality was observed between the two groups. Reduction within the number of days to resolution of ache, variety of days to resolution of belly tenderness, and duration of hospitalization had been noticed in the needle aspiration group only. This fast clinical response was particularly famous in these with larger (>6 cm) abscesses, and there have been no problems. The procedure resulted in decreased drainage in 48 hours, and in 11 of 13 patients the drainage catheter was removed by 1 week and after 10 days within the remaining two sufferers. Clinical improvement and important lower was noted in the quantity of the abscess cavity, and no recurrence of abscess was famous after 9 to 25 months of follow-up. Factors used to predict rupture include diameter 5 to 10 cm, progressive improve in size, and left lobe location. Amebic pericarditis accounts for 4% of all extraintestinal amebiasis, with a mortality rate of roughly 30%. For ruptured abscess, the mortality fee is reported to be from 6% to as high as 50%. Factors independently associated with poor consequence are elevated serum bilirubin (>3. In industrialized nations, danger groups embody male homosexuals, vacationers and recent immigrants, and institutionalized populations. Patients are also more prone to have a history of fever, right higher quadrant abdominal pain, and diarrhea. Surgical procedures are used for sufferers who fail these administration approaches or expertise issues of the abscess, similar to peritoneal rupture or empyema. Prevention efforts would come with enchancment of sanitation and hygiene and use of protected sexual practices. Vaccination strategies particularly with recombinant antigens are being studied as nicely. Single and multiple pyogenic liver abscesses: etiology, clinical course, and end result. Clinical course, therapy, and multivariate analysis of threat components for pyogenic liver abscess. Pyogenic liver abscess: does Escherichia coli trigger extra antagonistic outcomes than Klebsiella pneumoniae Clinical and radiological features of invasive Klebsiella pneumoniae liver abscess syndrome.
Purchase zestoretic now
One hypothesis envisions the activation of pancreatic stellate cells, which induce desmoplasia, as the necessary thing pathogenetic "swap" that leads to the transition to continual pancreatitis. At a second assembly in Marseille held in 1984,2,three continual pancreatitis was subclassified as continual pancreatitis with focal or segmental or diffuse fibrosis, and chronic pancreatitis with or without stones, and obstructive chronic pancreatitis was listed as a distinct type. To help outline changes related to clinical threat elements, a 1988 meeting in Rome added the morphologic distinction of persistent calcifying pancreatitis, which is characterized by intraductal calcifications and protein plugs, and continual inflammatory pancreatitis, which is characterised by dense infiltration of mononuclear inflammatory cells. Moreover, no classification system has confirmed practical applicability in guiding selections for therapy. This article outlines the definition, risk elements, scientific manifestations, prognosis, and therapy options for the disease. Discussion of management choices contains an outline of medical, endoscopic, and surgical interventions. Different disease processes inflicting similar-appearing damage to the pancreas might comply with totally different medical programs. Thus, quite than classifying pancreatitis based on the presumed causative agent, Whitcomb et al. Patients with idiopathic illness sometimes fall right into a bimodal age distribution, presenting between the ages of 10 and 20 or after age 50 years. However, many of these sufferers are increasingly acknowledged to have underlying genetic mutations and polymorphisms and may be more appropriately recategorized into the genetic subgroup. The inheritance sample of hereditary persistent pancreatitis is autosomal dominant and has roughly a 78% penetrance fee. Genetic linkage evaluation established a locus for hereditary continual pancreatitis on chromosome 7q, a region that encodes eight completely different zymogen genes together with various trypsins and carboxypeptidase A. It is unknown if tobacco initiates the disease10; however, tobacco is believed to potentiate the progression. In a preclinical model, investigators demonstrated that tobacco exposure increases the danger of pancreatic cancer in persistent pancreatitis patients. The R122H mutation produces a proteolyticresistant trypsinogen favoring inappropriate activation throughout the pancreas, resulting in autodigestion. Variations in numerous other genes have been related to continual pancreatitis. The most frequent mutation associated with persistent pancreatitis is an N34S amino acid substitution in exon 3. More than a thousand mutations have been characterized with a wide range of impact on the characteristics of the channel function. The medical manifestations are depending on the particular mutation and the impact on the useful attribute of the chloride channel. Focal inflammation seen with this disease can typically mimic a pancreatic mass, which may be tough to differentiate from a pancreatic malignancy on imaging studies. This mechanism is poorly understood however doubtless entails the accumulated results of postinflammatory scarring and necrosis in addition to the priming of pancreatic stellate cells to induce fibrosis. In addition, radiation and ischemia may contribute to irreversible histopathologic changes and inflammation attribute of chronic pancreatitis. Causes of pancreatic obstruction include pancreatic or ampullary tumors, and postinjury pancreatic duct fibrosis. Elevated basal pressures on the sphincter of Oddi are thought by some to result in relative outflow obstruction from the proximal duct and thereby contribute to pancreatitis. Patients may also have anatomic variations within the pancreatic ductal system that predispose for obstruction, most notably pancreas divisum. However, the vast majority of sufferers with pancreas divisum are asymptomatic; thus, the anatomic variation could predispose to pancreatitis together with other threat elements. In some sufferers, particularly early in the course of the disease, pain could additionally be a minor characteristic. The pain is most incessantly localized to the epigastrium, often radiates to the back, and is typically associated with nausea and vomiting. Between 4% and 30% of sufferers have significant exocrine insufficiency and report bloating, flatulence, or steatorrhea. Malabsorption leads to weight loss and deficiencies in micronutrients, especially fatsoluble nutritional vitamins A, D, and E.
Purchase zestoretic without prescription
Perioperative and late clinical outcomes of percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. Stenting of stenotic mesenteric arteries for symptomatic continual mesenteric ischemia. Comparison of covered stents versus bare steel stents for treatment of chronic atherosclerotic mesenteric arterial illness. Endovascular repair of chronic mesenteric occlusive disease: the function of duplex surveillance. Type 1, or graft-enteric fistula, happens as the end result of an erosion of the proximal aortic suture, with or with out the presence of a pseudoaneurysm, into the adjacent bowel. Failure to close the aneurysm sac and retroperitoneum may even go away the suture line in direct contact with the duodenum, increasing the percentages of abrasion of the suture line into the bowel. Foreign-body ingestion, carcinoma, or infections similar to diverticulitis can lead to adhesions that deliver the bowel in closer proximity to the aorta. The mechanical pulsations cause thinning of the bowel wall with eventual translocation of enteric organisms into the suture line. The higher chance of a fistula forming between the aorta and duodenum is attributed to their proximity to each other, because the duodenum directly overlies the aorta inside the retroperitoneum. The analysis is often delayed due to the rarity of the illness and the extensive differential that accompanies the preliminary mild symptoms. Patients with this prognosis have a grim prognosis, and surgery is the only truly definitive management possibility. Intermittent herald bleeds in the type of hematochezia, melena, or hematemesis are common occurrences, being current in 94% of circumstances. Laboratory Studies Laboratory studies could demonstrate abnormalities, such as an elevated white blood cell depend and decreased hematocrit. In the presence of fever, aerobic and anaerobic blood cultures ought to be obtained. Advanced sepsis confirmed by optimistic preoperative blood cultures is a predictor of poor end result. The most typical organisms isolated from the fistula site embrace Staphylococcus aureus (including methicillin-resistant S. A hemodynamically unstable affected person should bear resuscitation whereas being prepped for an emergency exploratory laparotomy. Indeed, the exploratory laparotomy is the gold standard, with one hundred pc sensitivity and specificity. If the affected person is stable, additional diagnostic checks must be obtained without delay. Periaortic gasoline, fluid, and gentle tissue edema also may be observed with graft infections and are normal findings instantly after the operation. Computed tomography scan reveals aortoenteric fistula between the aortic graft and the third portion of the duodenum. Increased sign intensity in T1- and T2-weighted images indicates localized irritation, and perigraft fluid seen after the preliminary postoperative interval might sign a graft infection. If the affected person is hemodynamically unstable, an arterial line and central line should be placed and rapid resuscitation initiated whereas getting ready the patient for an exploratory laparotomy. The affected person must be typed and crossmatched and obtain empiric intravenous broad-spectrum antibiotics that cover both gram-positive and enteric organisms. In steady sufferers, a diagnostic work-up may be initiated with a comprehensive operative plan set in place. Because good visualization of the surgical field is essential, the initial must be performed in the working room, in the event of a catastrophic hemorrhage. Endoscopy might reveal a portion of the graft protruding into the bowel, lively bleeding, ulcerations, petechiae, blood clot, or extrinsic pulsating mass. Plain belly radiographs might show pneumoperitoneum from the perforated bowel and could be one of many first indicators that alert the clinician to the severity of the situation. Proximal and distal management of the aorta is crucial previous to manipulation of the fistula website to prevent uncontrollable hemorrhage.
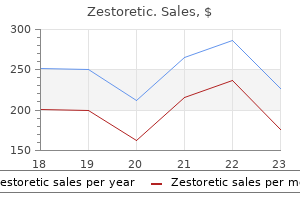
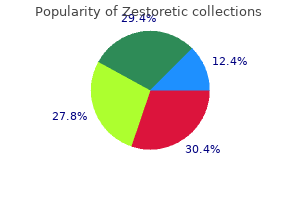
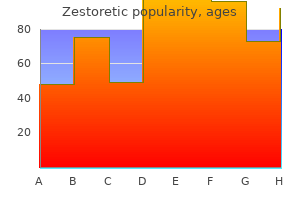
Real Experiences: Customer Reviews on Zestoretic
Randall, 61 years: In the syndromatic situation, the seek for related anomalies contains consultation by ophthalmology, cardiology, nephrology, and gastroenterology. Comparison of two doses of imatinib for the remedy of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 sufferers.
Brant, 45 years: Cholesterol polyps are the commonest of the benign tumors, accounting for approximately 60% of all gallbladder polyps. The anastomosis is often carried out with interrupted sutures in a single layer.
9 of 10 - Review by A. Tuwas
Votes: 67 votes
Total customer reviews: 67

